Nurses step up in crises
Kaiser Permanente nurses have been saving lives on the front lines since 1942.
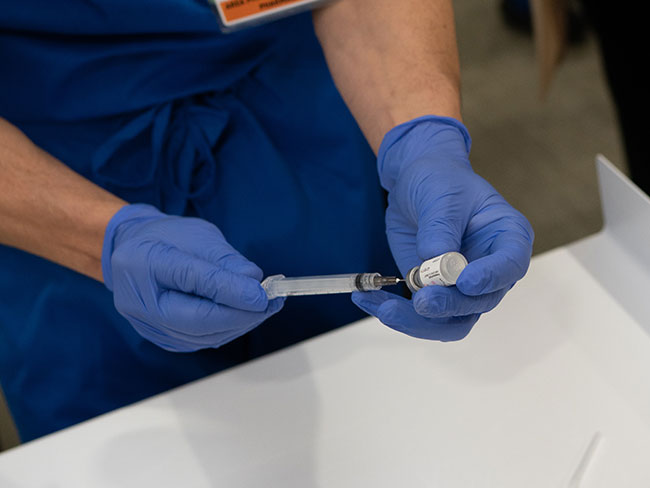
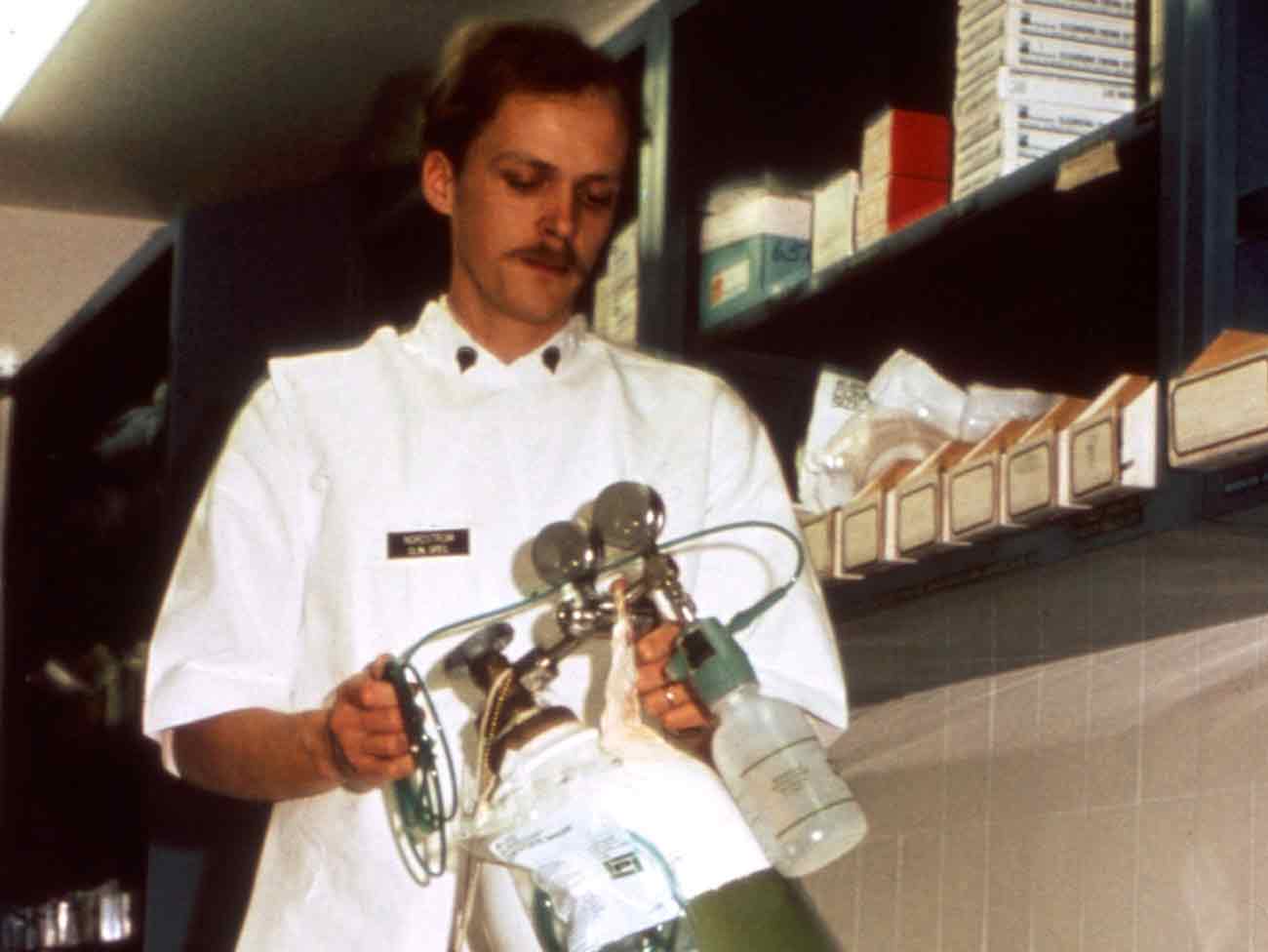
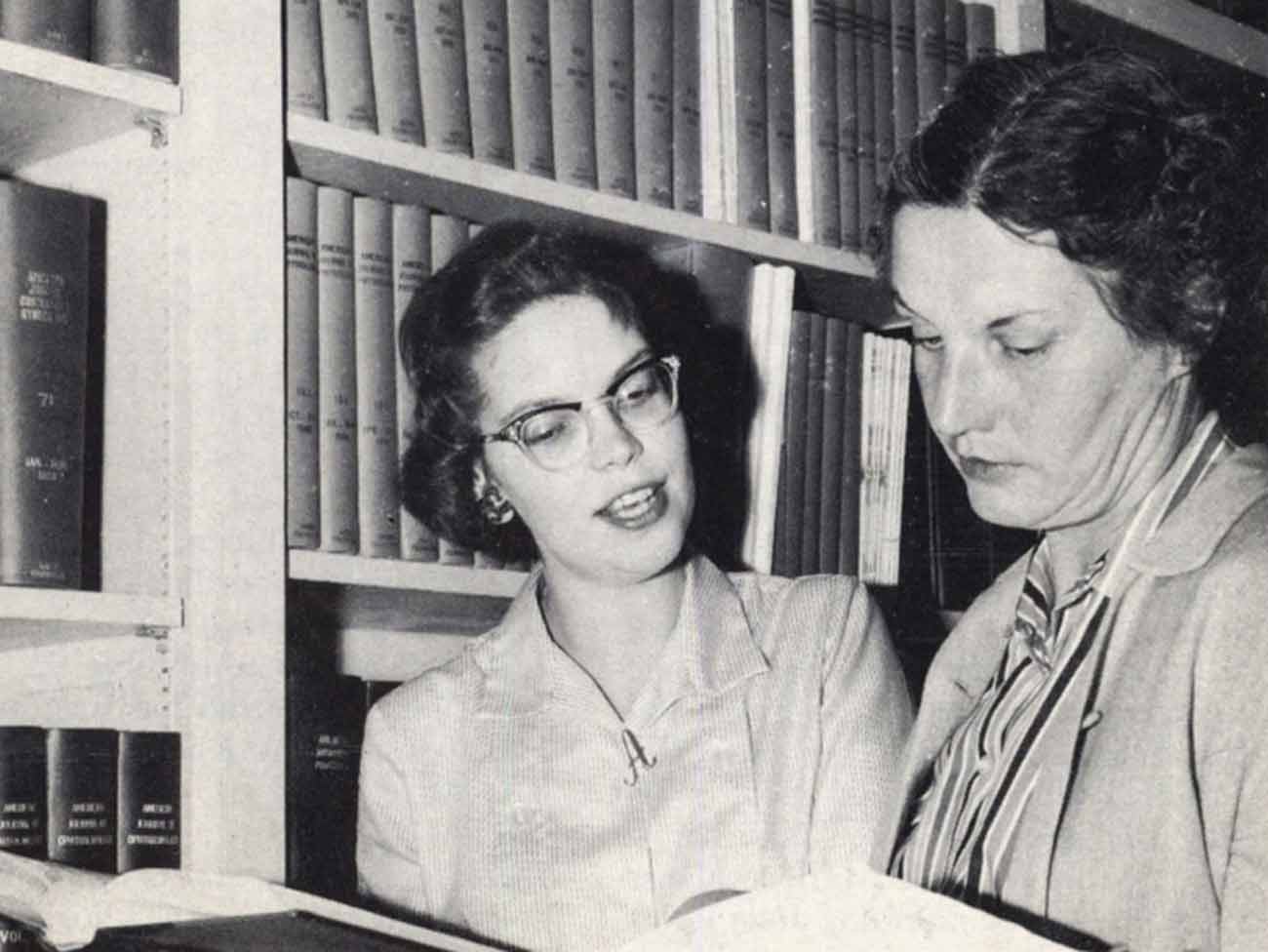
Laboratory personnel at Kaiser Permanente San Francisco Medical Center listening to AIDS training by Barbara Lamberto, RN, infection control coordinator. (The Reporter, September 1983)
The COVID-19 pandemic is not the first time Kaiser Permanente nurses have stepped up to meet extreme health emergencies. Time after time throughout the organization’s 75-year history, nurses have met crises with skill, compassion, and courage.
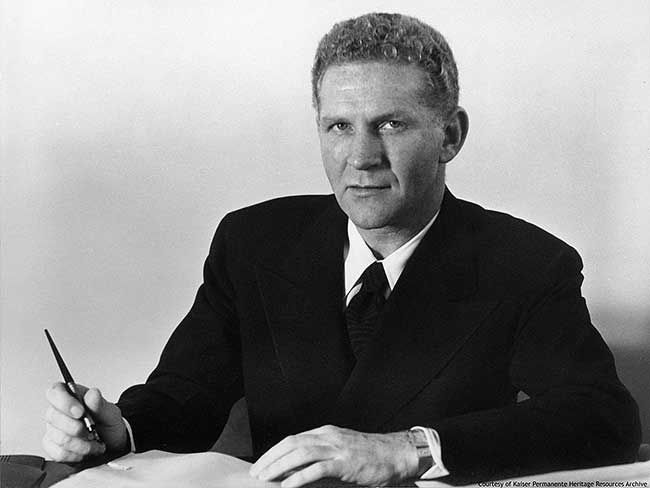
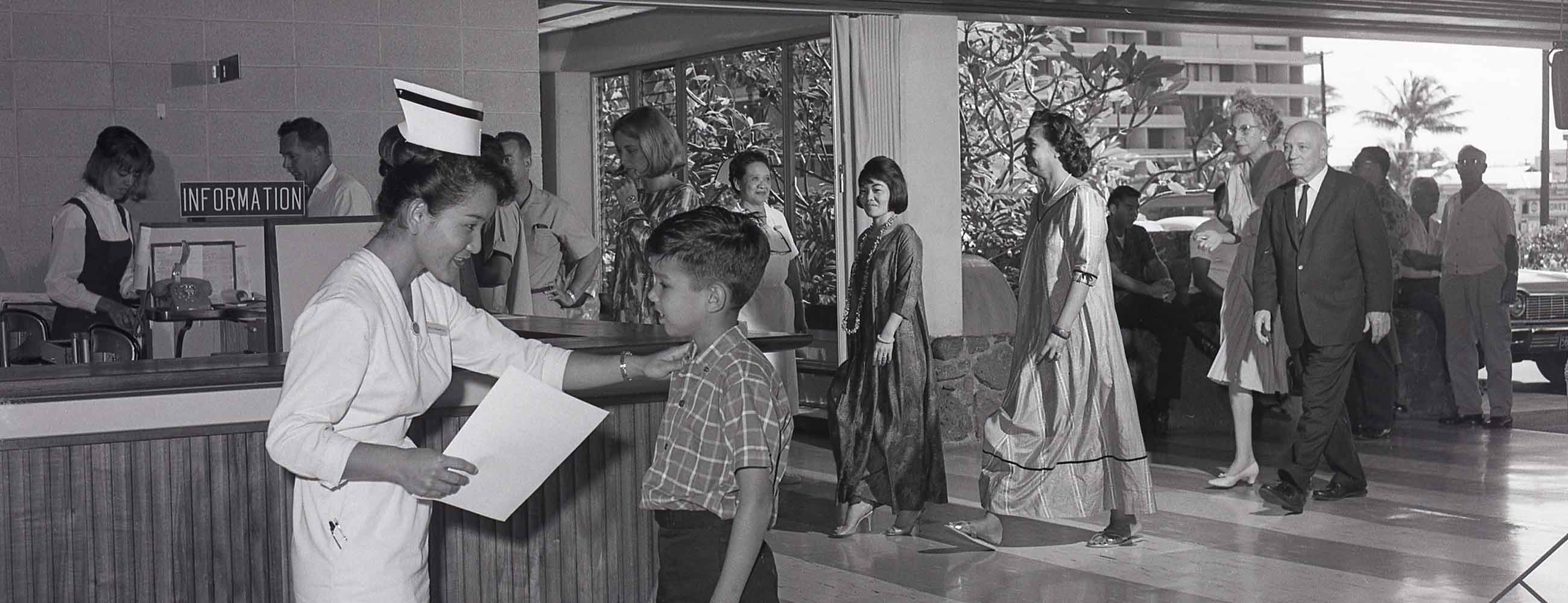
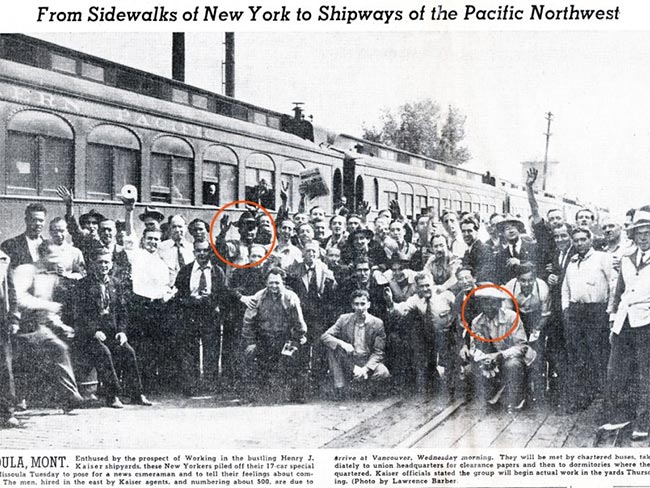
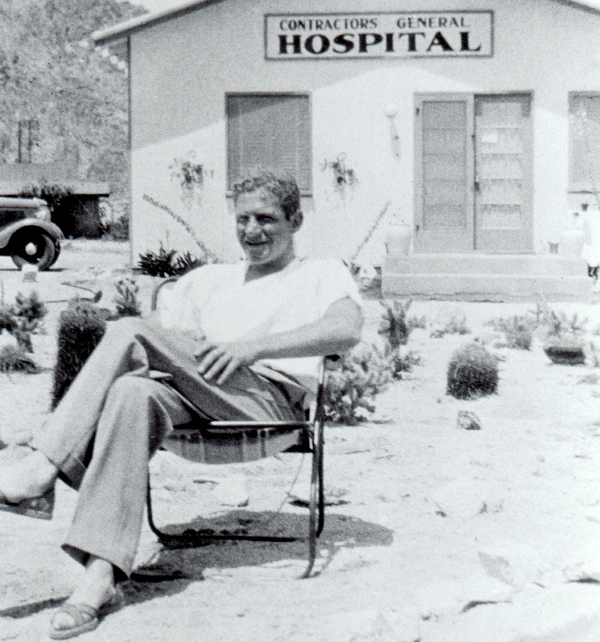
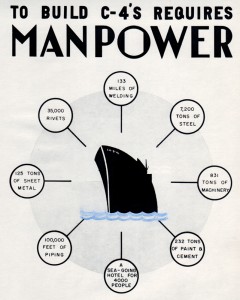
When the Permanente Health Plan was formed to serve Henry J. Kaiser’s shipyard workers at the beginning of World War II, our founding nurses found themselves dealing with an ever-growing patient load, an overwhelming number of industrial injuries, and limited resources. During the home-front challenges, the Richmond Field Hospital and the main Permanente Foundation Hospital in Oakland were constantly jammed and expanding. Registered nurse Clair Lisker recalled that, even after the war ended and the health plan opened to the public, we were so busy we would have patients out in the hallways, lined up, because we didn’t have enough bed space in the patients’ rooms.
Until COVID-19 appeared, unquestionably the organization’s biggest challenge was the AIDS epidemic of the late 1980s and early 1990s. AIDS was a mysterious and terrifying disease that traumatized patients and caregivers alike. No one knew what protocols to follow. Nurses were crucial to our effective and culturally competent response.
In 1983, Marianne Bond was an infection control nurse at Kaiser Permanente San Francisco Medical Center. Frustrated by the lack of protocols, she developed a 30-minute in-service training on patient-caregiver precautions based on what she’d learned about hepatitis B transmission. Registered nurse Barbara Lamberto, infection control coordinator at that facility, was quoted in the employee magazine Spectrum: "As health care workers, it's important to put things in perspective — to educate ourselves about the realities of the disease and then to replace our fears with compassion."
Before more progressive visitation policies were established during the AIDS crisis, significant others did not have the same rights as family members. Nurses were the gatekeepers who controlled visitation rights for dying patients without blood relatives or family, and they made allowances. Their actions informed the creation of updated policies that expanded hospital visitation rights for significant others.
AIDS taught many lessons. In the summer of 1987, the Kaiser Permanente employee magazine Spectrum published a summation by Neil Schram, MD, an internist at Southern California's Kaiser Foundation Harbor Hospital "This virus won't conform to our rules, and we'd better face that fact by finding new ways to adapt and cope. Because it's not going away."
Not to be lost in the impact of the AIDS epidemic was the handling of another public health challenge, hepatitis.
Hepatitis A blossomed into an epidemic in 1985, and by the fall, 75 people in Sacramento County, California, had died of this virus. The crucial step of tracking the community spread was baffling epidemiologists. But Angie Merrill, an infection control nurse at the Kaiser Foundation Hospital in Sacramento, collaborated with a counterpart at Sacramento’s University Medical Center, a location that had also experienced an outbreak. Frustrated at failing to find links between cases at the 2 facilities, Merrill had an “Eureka!” insight. She later recounted, "They're doughnut people. They eat doughnuts with coffee every morning in the cafeteria." And yes, both facilities shared a common doughnut vendor. Her finding solved the case.
These health crises were followed by others: anthrax in 2001, H1N1 in 2009, Ebola in 2014, and now COVID-19 and its impact in 2020. In every instance — from 1942 through today — Kaiser Permanente nurses have been on the front lines saving lives, innovating, and demonstrating extraordinary leadership.

July 16, 2025
A new gold standard in nursing excellence
Woodland Hills Medical Center is our first hospital in Southern California …

April 30, 2025
A history of trailblazing nurses
Nursing pioneers lay the foundation for the future of Kaiser Permanente …

April 30, 2025
Celebrate National Nurses Week with me
Join us in honoring our nurses for their dedication to providing high-quality, …

April 30, 2025
Celebrating our extraordinary nurses
Our nurses are leaders and patient advocates. They transform care and improve …
April 16, 2025
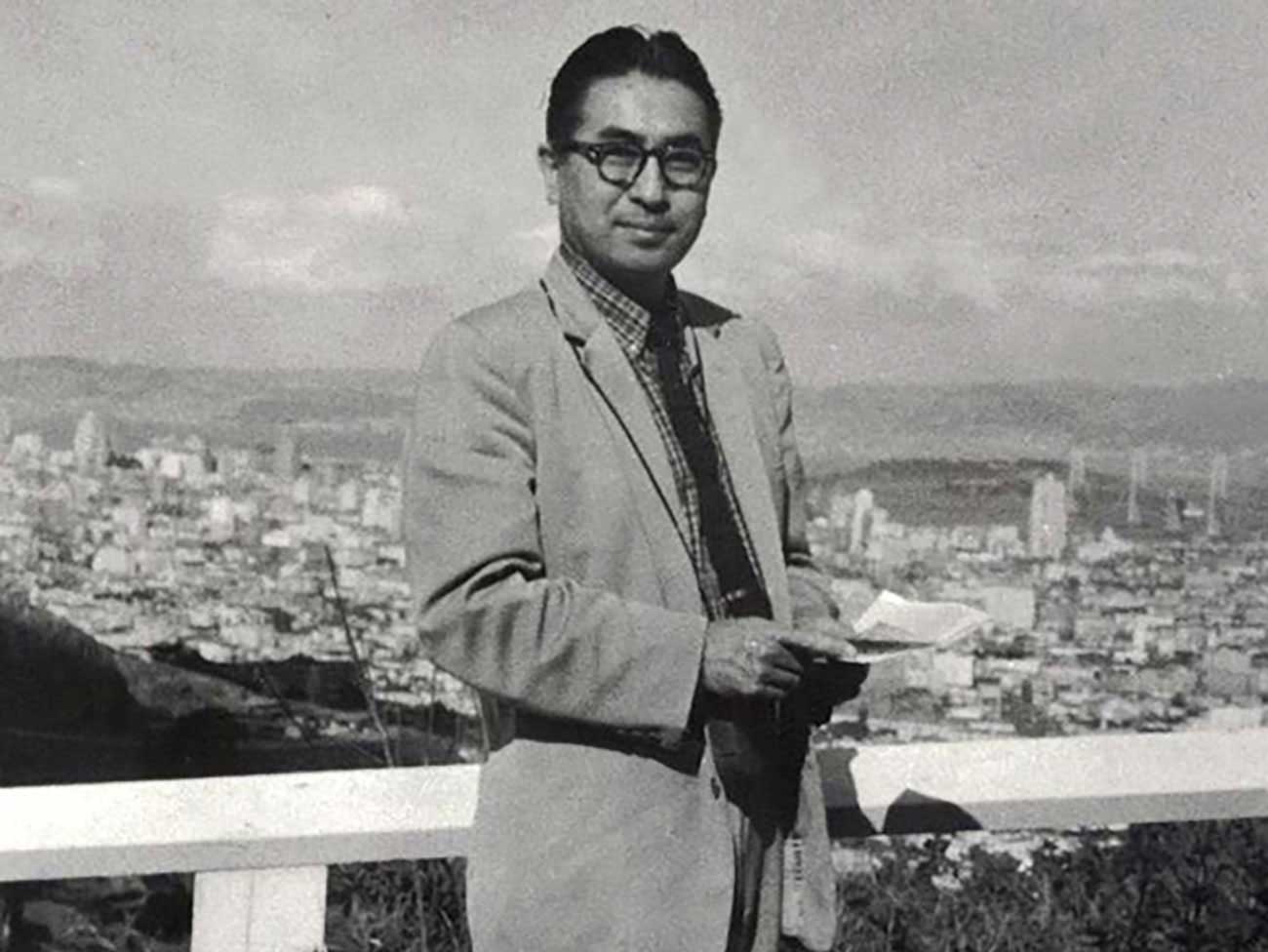
Sidney R. Garfield, MD: Pioneer of modern health care
Kaiser Permanente’s co-founding physician spread prepaid care and the idea …

February 24, 2025
Honoring extraordinary nurses
Our award-winning nurses put patients first and contribute new knowledge …

May 3, 2024
Henry J. Kaiser: America’s health care visionary
Kaiser was a major figure in the construction, engineering, and shipbuilding …

April 9, 2024
Building partnerships to inspire the next generation
Kaiser Permanente supports education and career opportunities for students …

April 8, 2024
Martin Luther King Jr.’s dream is alive at Kaiser Permanente
Greg A. Adams, chair and chief executive officer of Kaiser Permanente, …

February 13, 2024
A legacy of life-changing community support and partnership
The Kaiser Permanente Watts Counseling and Learning Center started as a …

February 2, 2024
Expanding medical, social, and educational services in Watts
Kaiser Permanente opens medical offices and a new home for the Watts Counseling …
October 17, 2023
How Kaiser Permanente evolved
Sidney R. Garfield, MD, and Henry J. Kaiser came together to pioneer an …

October 10, 2023
What to know about COVID-19 vaccines
The updated vaccine is recommended for everyone 6 months and older.

October 3, 2023
Nursing excellence recognized at Fontana Medical Center
The prestigious Magnet® designation affirms the compassion, dedication, …

September 13, 2023
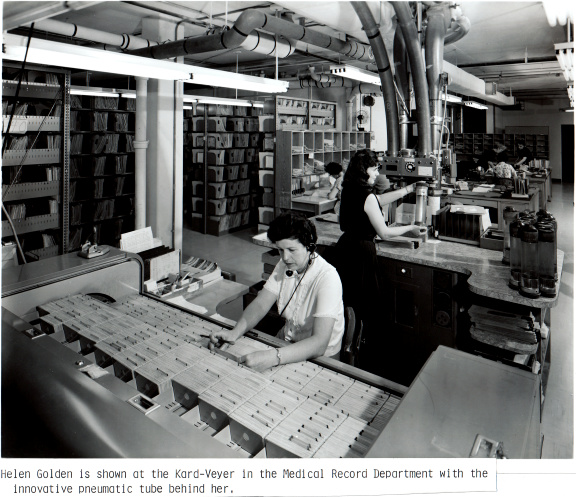
Transforming the medical record
Kaiser Permanente’s adoption of disruptive technology in the 1970s sparked …

August 17, 2023
Beyond clinic walls: Research supporting healthy communities
Stories in the Department of Research & Evaluation 2022 Annual Report demonstrate …

August 15, 2023
'Hot-spot' strategy gets more Californians vaccinated
A new location-based vaccine strategy by Kaiser Permanente was successful …

August 8, 2023
Nursing excellence: Joining the elite 10% in the nation
Kaiser Permanente Panorama City Medical Center achieves coveted Magnet® …

May 18, 2023
The gold standard of nursing excellence
Kaiser Permanente Baldwin Park Medical Center achieves Magnet status, the …

May 16, 2023
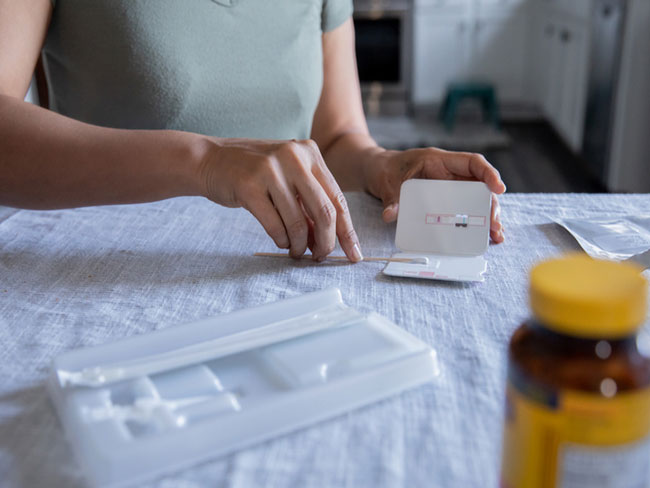
COVID-19 public health emergency has ended: What’s changed?
Vaccinations, testing, and treatment are still widely accessible. Member …
May 11, 2023
COVID-19 testing, testing — Get results in 1, 2, 3
Testing is the most important way you can help control the spread of COVID-19.

May 2, 2023
Women lead an industrial revolution at the Kaiser Shipyards
Early women workers at the Kaiser shipyards diversified home front World …

April 25, 2023
Hannah Peters, MD, provides essential care to ‘Rosies’
When thousands of women industrial workers, often called “Rosies,” joined …

April 11, 2023
Collaboration is key to keeping people insured
With the COVID-19 public health emergency ending, states, community organizations, …
November 11, 2022
A history of leading the way
For over 75 innovative years, we have delivered high-quality and affordable …
November 11, 2022
Pioneers and groundbreakers
Learn about the trailblazers from Kaiser Permanente who shaped our legacy …
November 11, 2022
Our integrated care model
We’re different than other health plans, and that’s how we think health …
November 11, 2022
Our history
Kaiser Permanente’s groundbreaking integrated care model has evolved through …
October 14, 2022
Contact Heritage Resources
October 1, 2022
Innovation and research
Learn about our rich legacy of scientific research that spurred revolutionary …

May 26, 2022
Nurse practitioners: Historical advances in nursing
A doctor shortage in the late 1960s and an innovative partnership helped …

November 30, 2021
Bechara Choucair, MD, returns as chief health officer
After serving on the White House COVID-19 response team, Bechara Choucair, …
October 12, 2021
Beyond advocacy: Requiring vaccination to stop COVID-19
Kaiser Permanente and other leading companies are mandating COVID-19 shots …

September 10, 2021
‘Baby in the drawer’ helped turn the tide for breastfeeding
This innovation in rooming-in allowed newborns to stay close to mothers …

August 25, 2021
Kaiser Permanente’s history of nondiscrimination
Our principles of diversity and our inclusive care began during World War …

July 22, 2021
A long history of equity for workers with disabilities
In Henry J. Kaiser’s shipyards, workers were judged by their abilities, …
June 2, 2021
Path to employment: Black workers in Kaiser shipyards
Kaiser Permanente, Henry J. Kaiser’s sole remaining institutional legacy, …

March 11, 2021
Our support of the American Rescue Plan Act
A statement from CEO Greg A. Adams about the American Rescue Plan Act.

February 22, 2021
The Permanente Richmond Field Hospital
Forlorn and all but forgotten, it played a proud role during the World …

September 28, 2020
A legacy of disruptive innovation
Proceeds from a new book detailing the history of the Kaiser Foundation …
August 26, 2020
Kaiser Permanente’s pioneering nurse-midwives
The 1970s nurse-midwife movement transformed delivery practices.
July 30, 2020
Books and publications about our history
Interested in learning more about the history of Kaiser Permanente and …
November 8, 2019
Swords into stethoscopes — veterans in health professions
Kaiser Permanente has actively hired veterans in all capacities since World …
August 28, 2019
When labor and management work side by side
From war-era labor-management committees to today’s unit-based teams, cooperation …

August 2, 2019
Thriving with 1960s-launched KFOG radio
Kaiser Broadcasting radio connected listeners, while TV stations brought …

June 5, 2019
Breaking LGBT barriers for Kaiser Permanente employees
“We managed to ultimately break through that barrier.” — Kaiser Permanente …

March 29, 2019
Equal pay for equal work
Kaiser shipyards in Oregon hired the first 2 female welders at equal pay …

February 5, 2019
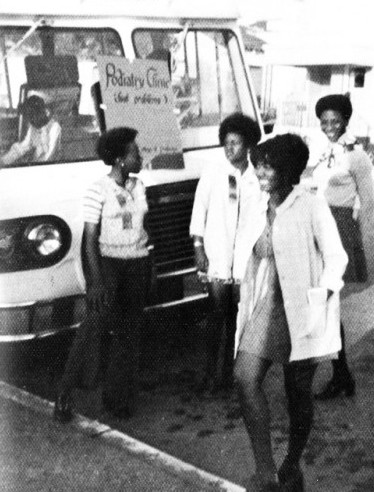
Mobile clinics: 'Health on wheels'
Kaiser Permanente mobile health vehicles brought care to people, closing …
December 10, 2018
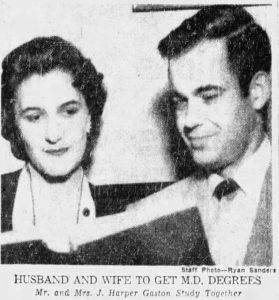
Southern comfort — Dr. Gaston and The Southeast Permanente Medical Group
Local Atlanta physicians built community relationships to start Kaiser …
May 30, 2018
John Graham Smillie, MD, pediatrician and innovator
Celebrating the life of a pioneering pediatrician who inspired the baby …

April 30, 2018
Nursing pioneers leads to a legacy of leadership
Kaiser Foundation School of Nursing students learned a new philosophy emphasizing …

April 19, 2018
Wasting nothing: Recycling then and now
Environmentalism was a common practice at the Kaiser shipyards long before …

April 12, 2018
Harold Hatch, health insurance visionary
The founding of Kaiser Permanente's concept of prepaid health care in the …
March 26, 2018
5 physicians who made a difference
Meet 5 outstanding doctors who advanced the practice of medical care with …

March 13, 2018
Henry J. Kaiser and the new economics of medical care
Kaiser Permanente’s co-founder talks about the importance of building hospitals …

March 8, 2018
Slacks, not slackers — women’s role in winning World War II
Women who worked in the Kaiser shipyards helped lay the groundwork for …

February 22, 2018
The amazing true story of Park Ranger Betty Reid Soskin
She is the oldest national park ranger in the country with a legacy of …
December 19, 2017
From boats to books: A history of Kaiser Permanente’s medical libraries
Kaiser Permanente librarians are vital in helping clinicians remain updated …

November 7, 2017
Patriot in pinstripes: Honoring veterans, home front, and peace
Henry J. Kaiser's commitment to the diverse workforce on the home front …

October 12, 2017
An experiment named Fabiola
Health care takes root in Oakland, California.

September 29, 2017
Harbor City Hospital: Beachhead for labor health care
The story of Kaiser Permanente's South Bay Medical Center finds its roots …

August 15, 2017
Sidney R. Garfield, MD, on medical care as a right
Hear Kaiser Permanente’s physician co-founder talk about what he learned …

August 10, 2017
‘Good medicine brought within reach of all'
Paul de Kruif, microbiologist and writer, provides early accounts of Kaiser …

July 14, 2017
Kaiser’s role in building an accessible transit system
Harold Willson, an employee, and an advocate for accessible transportation, …

July 7, 2017
Mending bodies and minds — Kabat-Kaiser Vallejo
The expanded new location provided care to a greater population of members …
June 23, 2017
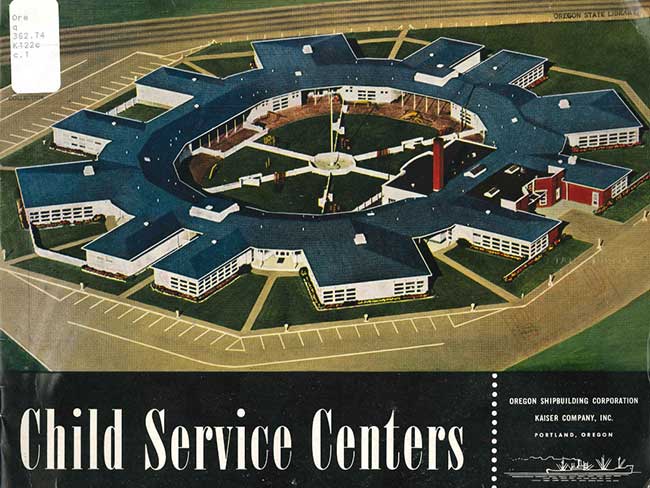
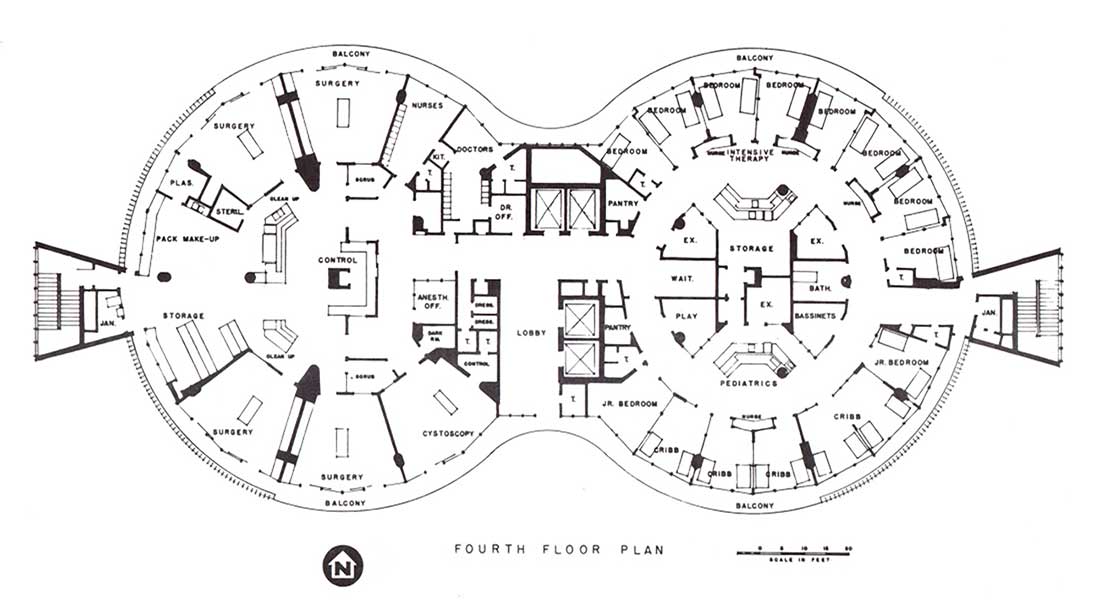
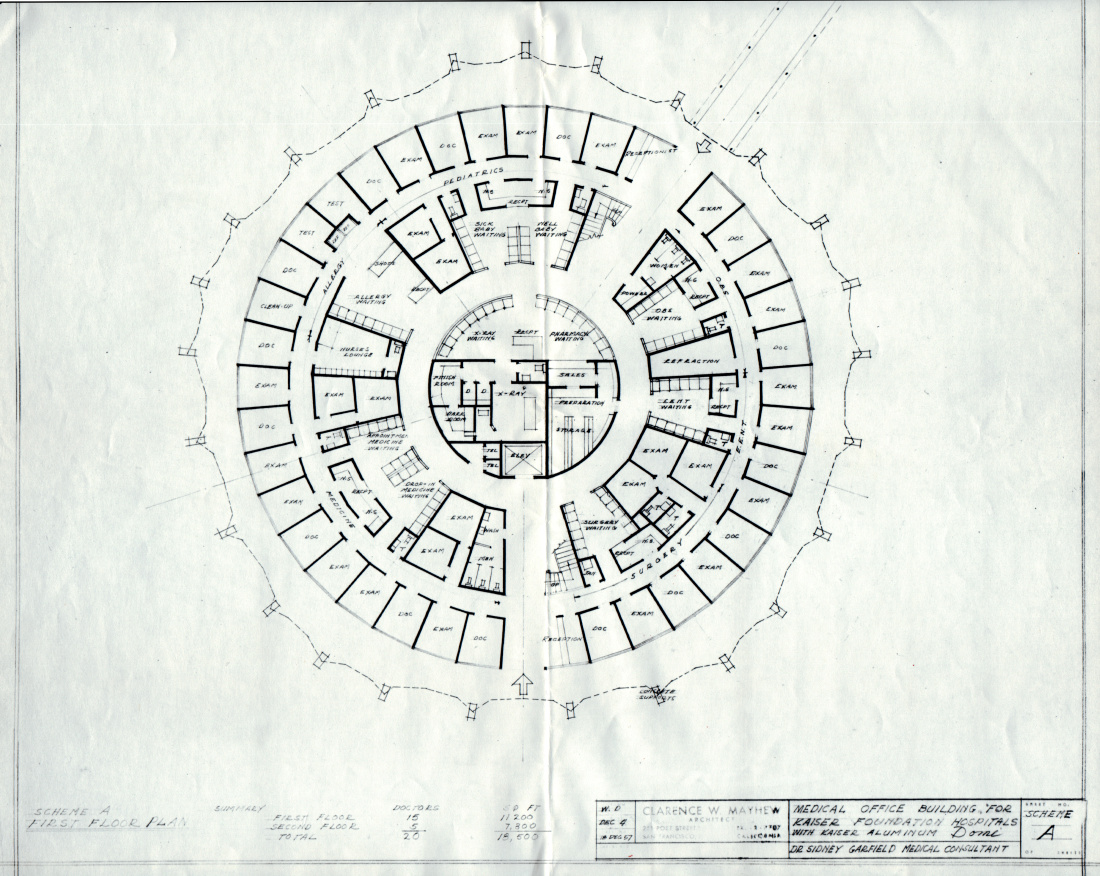
No getting round it: An innovative approach to building design
Kaiser Permanente incorporated innovative circular architectural designs …

June 14, 2017
Kabat-Kaiser: Improving quality of life through rehabilitation
When polio epidemics erupted, pioneering treatments by Dr. Herman Kabat …

June 9, 2017
Edmund (Ted) Van Brunt, pioneer of electronic health records, dies at age …
Throughout his career, Dr. Van Brunt applied computers and databases in …

May 4, 2017
How a Kaiser Permanente nurse transformed health education
Kaiser Permanente's Health Education Research Center and Health Education …

March 22, 2017
Kaiser Permanente and Group Health Cooperative: Working together since …
The formation of Kaiser Permanente Washington comes from longstanding collaboration, …

March 7, 2017
Beatrice Lei, MD: From Shantou, China, to Richmond, California
She served as a role model and inspiration to the women physicians and …
March 1, 2017
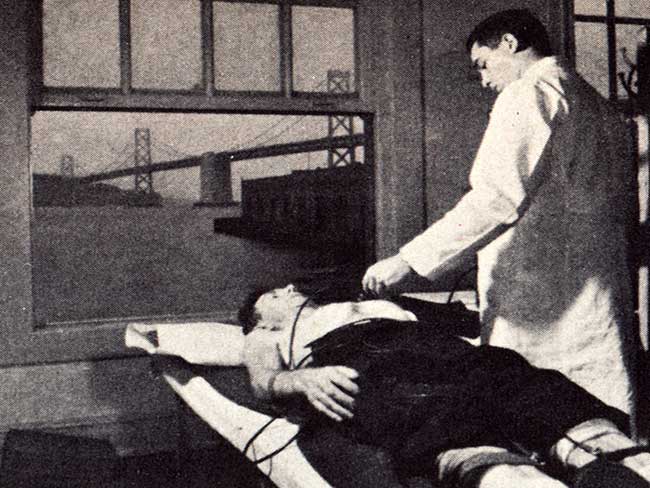
Screening for better health: Medical care as a right
When industrial workers joined the health plan, an integrated battery of …
February 17, 2017
Experiments in radial hospital design
The 1960s represented a bold step in medical office architecture around …

February 3, 2017
Ellamae Simmons — trailblazing African American physician
Ellamae Simmons, MD, worked at Kaiser Permanente for 25 years, and to this …
January 27, 2017
Japanese-American doctors overcame internment setbacks
Despite restrictive hiring practices after World War II, Kaiser Permanente …

November 16, 2016
Betty Reid Soskin honored with lifetime achievement award
The California Studies Association presents the Carey McWilliams Award …

October 17, 2016
Kaiser Motors in Oakland — “We sell to make friends.”
In 1946 Henry J. Kaiser Motors purchased half a square block in downtown …
October 12, 2016
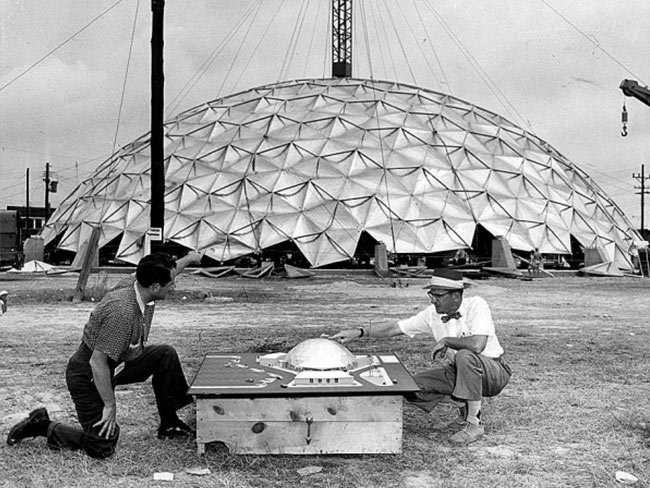
Kaiser’s geodesic dome clinic
There are hospital rounds, and there are round hospitals.

May 5, 2016
Male nursing pioneers
Groundbreaking male students diversify the Kaiser Foundation School of …
April 20, 2016
Henry J. Kaiser’s environmental stewardship
Since the 1940s, Kaiser Industries and Kaiser Permanente have a long history …
November 13, 2015
Dr. Morris Collen’s last book on medical informatics
The last published work of Morris F. Collen, MD, one of Kaiser Permanente’s …
October 29, 2015
From paper to pixels — the new paradigm of electronic medical records
Transitioning to electronic health records introduced new approaches, skills, …

September 23, 2015
Kaiser Permanente and NASA — taking telemedicine out of this world
Kaiser Permanente International designs, develop, and test a remote health …
July 22, 2015
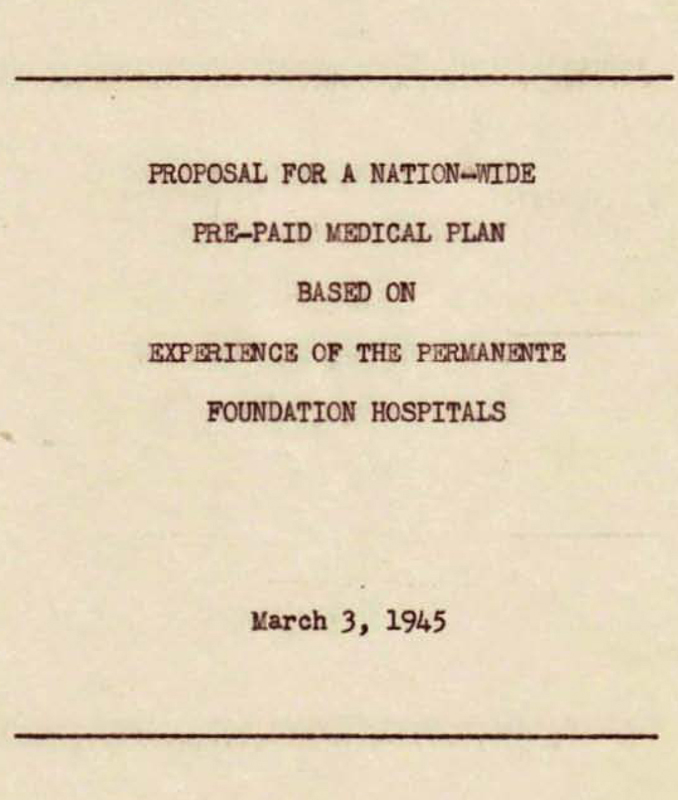
Kaiser Permanente as a national model for care
Kaiser Permanente proposed a revolutionary national health care model after …
July 21, 2015
Kaiser Permanente's early support from labor
Experiencing the Kaiser Permanente health plan led labor unions to support …
July 20, 2015
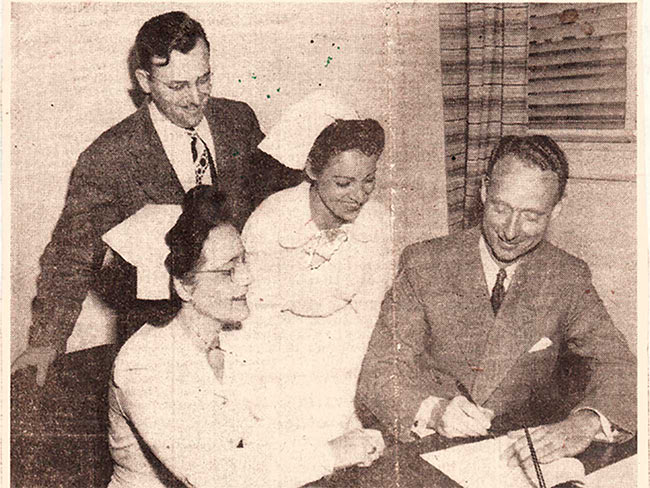
Opening the Permanente plan to the public
On July 21, 1945, Henry J. Kaiser and Dr. Sidney Garfield offered the health …

July 1, 2015
Sculpture dedicated to Kaiser Nursing School
The Kaiser Foundation School of Nursing sculpture near Kaiser Oakland hospital …

May 6, 2015
Celebrating Betty Runyen — Kaiser Permanente’s ‘founding nurse’
In a desert hospital during the Great Depression, Betty Runyen overcame …

April 27, 2015
Eugene Hickman, MD — Pioneering Black physician
Dr. Hickman had a long career at Kaiser Permanente, becoming president …

April 24, 2015
2 historical reflections on Kaiser Permanente
April 2, 2015
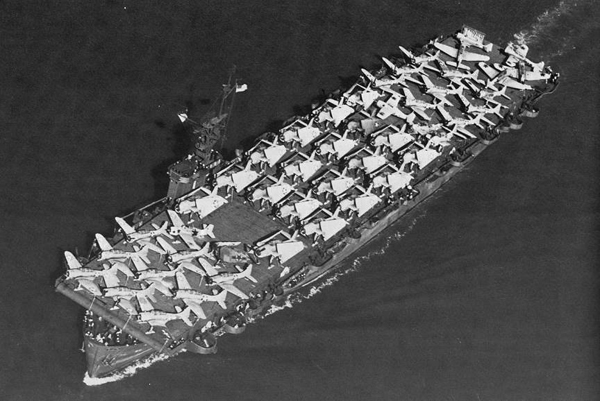
Henry Kaiser’s escort carriers and the Battle of Leyte Gulf
January 9, 2015
The World War II Kaiser Richmond shipyard labor force

December 16, 2014
Henry J. Kaiser on veteran employment and benefits
December 11, 2014
Henry J. Kaiser, geodesic dome pioneer

July 23, 2014
Kaiser shipyards pioneered use of wonder drug penicillin
Though supplies for civilians were limited, Dr. Morris Collen’s wartime …
June 24, 2014
Kaiser Permanente's first hospital changes and grows
A collection of vintage photos that chronicle the evolution of Oakland …

June 20, 2014
Old hospital holds memories of Kaiser Permanente’s past
Rebuilt Oakland Medical Center to open for business.

May 13, 2014
Henry J. Kaiser sticks up for union labor at Brewster Aeronautical
May 5, 2014
Black nurses get together to forge their own future
California African American nurses organize in early 1970s to address health …

May 1, 2014
Beloved nurse earned place in Kaiser Permanente history
Jessie Cunningham, the first Black nursing supervisor at Oakland Medical …