Celebrating our extraordinary nurses
Our nurses are leaders and patient advocates. They transform care and improve health for our members and communities.
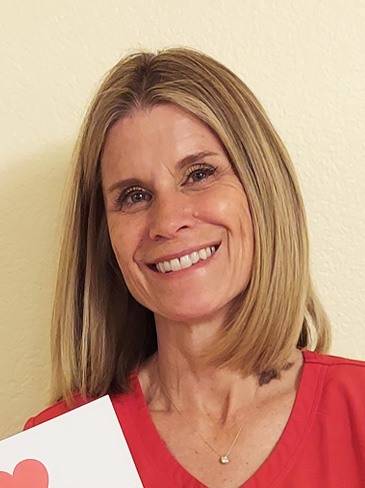
Carol Buhler (left) and Jaclyn Montano (right) are a mother-daughter nursing duo that spans 2 generations of Kaiser Permanente care.
more about nurses week
At Kaiser Permanente, we have a strong team of 76,000 nurses, ready to deliver high-quality, evidence-based care. Our nurses build on the work of those before them and set the standard for the future of nursing. In honor of Nurses Week, we thank them.
These 9 profiles show the many ways our nurses use best practices and new evidence to transform patient care. They also show the close relationships that nurses form through their teamwork and collaboration. In some cases, they are — quite literally — family.
One big happy family
Carol Buhler, RN, is a senior nurse manager at our appointment and advice call center in Sacramento, California. She delivered her daughter, Jaclyn Montano, a twin, at a Kaiser Permanente hospital. Montano now also works as a Kaiser Permanente nurse.
Jaclyn Montano, RN, works in the intensive care unit at our Roseville Medical Center, in Roseville, California.
The mother-daughter duo spans 2 generations of Kaiser Permanente nursing and care.
Buhler first interviewed for a nursing position at Kaiser Permanente in 1982. Soon after beginning work, Buhler went into early labor.
She safely delivered her twins at a Kaiser Permanente hospital.
The twins spent 30 days in intensive care. Their care team followed their progress closely for a year.
“Kaiser Permanente saved their lives. I will always be grateful,” Buher said between tears.
Montano has a care story of her own. At age 8, Montano’s eldest daughter was diagnosed with leukemia. She received treatment at our Roseville Medical Center, in Roseville, California. “They saved my child’s life,” Montano said.
Her daughter is now healthy and excelling in her high school life.
Buhler: The appointment and advice call center first began as a project in 1997 that served the Sacramento area. We evolved into what we call a “virtual medical center” in 2024. We now take calls and provide telehealth services to members from anywhere, even members who call while on vacation in Italy.
The biggest difference is the member experience. KP now offers direct lines to various clinicians 24/7.
Montano: We’re always seeking to improve our practice, our own professional development, and our patient outcomes. Many of our nurses have certifications in specialty areas.
Our unit received the Beacon Award for nursing excellence this year. The national award recognizes exceptional patient care in a healthy work environment. Each award is valid for 3 years.
Buhler: It’s the extraordinary care that Kaiser Permanente provides. The services are all here. My team is close and supportive of each other. We also have support of such good leaders. I think it’s the best place to work.
Montano: I always intended on ending up here because of Kaiser Permanente’s values. It’s a full-circle moment for me because we focus on the whole person and take care of the patient for the span of their entire life. My family is a living, multigenerational testament to that.
Excellence at work
Neelima Tigulla, RN, is a nurse manager of the medical-surgical units at our Orange County Anaheim Medical Center in Anaheim, California.
Under her leadership, the 2 hospital units she oversees have reduced pressure injuries and infections for several years by working together with multidisciplinary teams, clinical nurses, and champions who educate their peers on preventing pressure injuries in hospital patients.
One unit went from October 2019 to October 2024 without a single pressure injury. The second unit has had no pressure injuries since November 2022.
Tigulla’s nursing teams also reduced their number of catheter-associated urinary tract infections. They used the same strategy of training their peers to become champions of this work. In one unit, there have been no infections in nearly 6 years. In the second unit, which started the effort a few years later, there have been no infections in almost 3 years.
Our technology is state of the art. It makes managing patient care more efficient.
For example, we now use devices that resemble cell phones to scan medications that patients need in the hospital. This technology improves patient safety by serving as a double check that patients are receiving the correct medications.
Technology has also enabled virtual care to grow. We offer more services and more ways to get care.
Kaiser Permanente invests in your professional development. This is so significant and valuable. It allows nurses to enhance the care we provide to patients. I’ve personally experienced the difference in care and treatment as a patient myself.
Before becoming an employee, I was a Kaiser Permanente member. I received exceptional care during my pregnancy, which made me a loyal patient.
When I entered nursing school, I decided I would get my license and only apply to work at Kaiser Permanente. That’s exactly what I did, and I absolutely love it — I consider myself very fortunate.
It’s all in the family
Elizabeth Peper, RN, is a primary care nurse at our Longmont Medical Offices in Longmont, Colorado.
She’s also the granddaughter of a former board member of Kaiser Permanente.
“I grew up knowing Kaiser Permanente and hearing about Kaiser Permanente,” Peper said. “My grandpa was a board member. He was so proud of me for coming to work for Kaiser Permanente. He always loved Kaiser Permanente. He had it for his family.”
Now, Peper is proud to be part of a team that works together to meet the needs of its patients.
“We do what we call ‘creative access,’” she said. “It’s a big team effort. We try to meet patients where they are.”
Here’s an example of how “creative access” works:
- A patient came in with his wife, who happened to fall right before his scheduled appointment. She commented on the fall during his appointment.
- Peper and the rest of the care team quickly stepped in to take the wife’s vital signs and assess her injuries.
- Another nurse scheduled a same-day doctor appointment for her.
- The quick care prevented a trip to emergency room.
“Everybody pitches in willingly to do their part,” Peper said.
Our electronic health record has advanced so much since I first started working at Kaiser Permanente. We’ve also broadened our geographic footprint in Colorado and spread through the state.
We have the confidence that our company is going to back us. We’re here for our members.
Before I came to work here, I read about the extraordinary patient care, for every patient, every time. Once I started working here, it felt like a pair of shoes that fit just right. We are so patient-centered.
Seeing patients heal is a reward
Suha Charney, RN, is a clinical nurse in orthopedics and podiatry at our Caton Hill Medical Center in Woodbridge, Virginia.
She cares for patients’ wounds and collaborates with other clinicians to provide optimal care to patients. She’s particularly proud of the work she does as the primary nurse in the lower limb clinic in the podiatry department.
As of 2022, patients who see a podiatrist can not only get basic wound care but also specialized attention from a nurse who can focus on podiatry wounds.
“The biggest reward is being able to see patients who have chronic wounds actually start to heal because they’re getting specialized care,” Charney said.
We can now give our patients access to things like minor surgical procedures in our outpatient clinic instead of in a hospital or an ambulatory surgery center.
For example, we opened a hand procedure clinic here in September 2024. We now perform procedures like carpal tunnel release and trigger finger release.
Offering more inpatient services makes care convenient and easy for patients. They can come to an environment where they know the doctor and the staff. They don’t have to coordinate an entire day off work.
Our integrated care approach makes a big difference. At Kaiser Permanente, integrated care means our doctors, nurses, specialists, and other care team members work together. And they’re all connected to each other — and our patients — by our electronic health record system.
It’s always a community effort. We have specialty staff who make it easier for me to do my job. I can get authorizations for patients quickly. I always know that I have people supporting what I’m doing.
I chose Kaiser Permanente because I had heard it was a company that invests in its employees through education resources, great benefits, and support from our leaders.
I’ve been able to complete my bachelor’s degree and earn my wound care certificate because of educational funding from Kaiser Permanente.
I also had a role model in my manager, who started working here as a clinical assistant and then earned a bachelor’s and a master’s degree. Climbing the ladder looked realistic to me.
Quicker follow-ups decrease risk
Becky Farinas, RN, is a primary care staff nurse at our Waipio Medical Office in Waipio, Hawaii.
She’s proud of her nursing team members and their efforts to decrease the number of people who visit the emergency room after receiving wound care.
She and her nursing team led a procedure change to call patients 2 weeks after their initial treatment instead of the usual 30 days. Her team also created a way for patients to connect with a nurse more easily after their initial care.
These changes started in January 2024. Since then, the number of patients who visited the emergency room for wound care dropped by 50%.
The practice has now been rolled out across Hawaii.
Patient care is always changing and improving. I’ve noticed that wound care has progressed from simple bandaging to more advanced techniques.
For example, we used to clean wounds with saline on a gauze pad. Then, we’d cover the wound with gauze moistened with saline and secure the gauze with a dry bandage.
But recent research has shown better ways to care for wounds. We now use various wound cleaning products, ointments, and advanced dressings.
Kaiser Permanente nurses are special because we all work together. Our well-organized approach to health care helps nurses communicate better and work together more efficiently. We can provide patient care that is more effective and efficient.
Also, we push each other to be better. In my department of 8 nurses, 6 have earned wound care certifications and 7 have earned ambulatory care certifications.
I choose to practice at Kaiser Permanente because we treat patients with compassion and respect, just like they’re part of our family.
I’m proud to work with a dedicated team that feels like a second family to me. I fully support our mission to provide high-quality care to our members, their families, and the communities we serve.
It takes a team
Kaitlyn Maib, RN, is an oncology infusion nurse at our Oncology Infusion Center in Tacoma, Washington.
She knows how important it is to have a team working together for the patient.
For example, Maib recently worked with several clinicians to improve care for a patient. The patient has a condition that prevents her body from making enough new blood cells. That meant the patient needed blood transfusions once or twice a week.
However, after consultations with her physicians, the patient started taking a medication that decreased her need for blood transfusions.
For 5 years, the patient had been receiving blood infusions through a long, thin tube inserted through a vein in her arm. This tube is called a PICC, or peripherally inserted central catheter.
“The oncologist started the medication process, and I was able to have the tough conversations with her and suggested that we talk to the doctor about removing the PICC line,” Maib said. “The patient couldn’t thank me enough for helping her understand the risks and benefits for getting that line out.”
Without the PICC line, the patient has more freedom of movement. And, she doesn’t have to come in for weekly dressing changes by a nursing team.
Patients have a lot more ways to get care now.
Today, a patient can schedule a phone call with their primary doctor or with a specialist. A patient can email their care team and get an answer that may lead to a video meeting.
It’s quicker than waiting for the next available appointment.
Our nurses work hard at developing and maintaining good relationships with other departments. That means when we need to coordinate care, we’re familiar with other departments’ processes. We can expedite patients’ needs and provide better care.
I really like the Kaiser Permanente model. I don’t have to go outside Kaiser Permanente to coordinate care from different specialties or departments.
There’s also better communication within departments, and things don’t get lost in translation. There’s more accountability of each department, and things don’t get missed.
Our electronic health record system also makes it easier to coordinate care and take care of patients.
Self-care is critical to success
Donnedria Coleman, RN, is a telehealth nurse for Kaiser Permanente in Georgia.
She’s part of a team that works together to improve patient care. One of the team’s projects is to make sure 60% of phone calls from members get answered within 60 seconds. In 2024, the team exceeded that goal by answering 87% of calls within 60 seconds.
The role of a telehealth nurse is demanding, Coleman says. You never know what kind of care needs your patients will have. That’s why she and her co-workers take care of their own well-being — they find it to be just as important as caring for patients.
Every month, her team does a virtual team-building activity that promotes good health. One activity promoted good nutrition and balanced meals for healthy eating. For 3 and a half months, nearly everyone on her team participated. At the end of the activity, more than half the team had made long-lasting changes. Taking care of themselves ensures optimal engagement at work and better care for our patients.
We’re on the cutting edge of technology. Over the years, we’ve gone from providing just face-to-face appointments to offering multiple ways to get care.
We can reach out to patients through a video call or chat through text messaging. We can use a messaging service to alert patients to critical lab results and request that they call the advice nurse. These changes help us provide high-quality care.
We work together as a cohesive unit. We’re also strong advocates for patients. We help patients communicate with doctors and make the care experience that much better.
I realized during the hiring process that preventive care and affordability are important issues. I thought, “This could be a great thing for me!”
As the years have gone by, I’ve also benefitted from top-notch compensation. The managers are approachable; I can go to them about anything.
In my experience, Kaiser Permanente is the best place to work.
In pursuit of excellence
Narlyn Llamas, RN, is a nursing professional development specialist at our Roseville Medical Center in Roseville, California.
She collaborated with other nurses to encourage 19 nurses in the Roseville area to complete a bachelor’s degree or higher and 49 nurses to earn professional board certifications in 2024. Llamas credits this achievement to all 13 nurses on the Professional Development Council, which she co-chairs with 2 other nurses.
She and the nurses on the council created preparation courses to support board certification. They also helped educate their peers. For example, they shared information on the value of education and on the tuition reimbursement that Kaiser Permanente offers.
“The nurses got used to seeing us come around,” Llamas said, “and it made them feel comfortable enough to ask other nurses they worked with, ‘When are you doing your bachelor’s degree?’ One of my passions is helping nurses advance.”
One of Llamas’ most impressive achievements was helping our Kaiser Permanente Roseville Medical Center earn Age-Friendly Health System recognition. This recognition, given by the Institute for Healthcare Improvement, recognizes medical facilities that are committed to following best practices in caring for older adults.
Llamas was the driving force behind the initiative to earn the recognition. She coordinated with geriatric resource nurses, local leaders, and stakeholders.
Since our region began its journey to help each one of our facilities achieve Magnet designation, the nurses have grown in so many ways. (Magnet designation, awarded by the American Nurses Credentialing Center, recognizes hospitals for nursing excellence.)
Now, more of our nurses ask questions about our existing practices. Nurses understand why they’re making changes in how they practice. Nurses also know how to find the right evidence to support the new changes. It all adds up to better patient care.
Nurses have all the resources they need to improve patient care. There’s so much support from our leadership to improve nursing.
We also have opportunities for professional growth. And, everyone is focused on providing high-quality care.
I’ve always wanted to work at Kaiser Permanente. The people I knew who worked at Kaiser Permanente were really happy. They said they liked the pay, the benefits, and the work ethic of their peers.
The patients I talked to before I came here also said they were very happy with the quality of care.
Life-saving treatment
Mandy Ellis, RN, is a pediatric advice nurse for Kaiser Permanente in Portland, Oregon.
She started at Kaiser Permanente as a medical assistant. After kidney damage from preeclampsia during her pregnancy, she got connected to specialty care through Kaiser Permanente. She was on dialysis during her last 2 terms as a nursing student and first year as a nurse.
“My kidney decline was gradual,” Ellis said. “By the time I was ready for a kidney transplant, I had started nursing school with a goal of earning my associate’s degree.”
The nursing school program was sponsored by Kaiser Permanente and The Ben Hudnall Memorial Trust. The Ben Hudnall Memorial Trust offers financial support and professional development resources to Kaiser Permanente nurses represented by the Labor Management Partnership.
The nursing school program accepted a total of 24 Kaiser Permanente employees. One of the program’s students turned out to be Ellis’ kidney donor.
They found each other after Ellis gave a presentation on her kidney disease during one of their classes.
“She literally came up to me right after class and took me to a private area. She said, ‘When the time comes, I want you to know I will give you my kidney.’ I went through my kidney transplant after completing nursing school and working for one year,” Ellis said.
Ellis went on to earn her bachelor’s degree also with the support of The Ben Hudnall Memorial Trust.
“I owe my life to my kidney donor — and indirectly to Ben Hudnall and Kaiser Permanente,” Ellis said.
We’ve advanced in lots of ways due to technology. When I first joined, we used to keep patient health records in paper charts. Our electronic health record system makes it easier to help patients with resources. For example, in our system, it’s easy to refer a patient in need of social services to a medical social worker.
I value having access to mental health and wellness specialists for pediatrics. I feel like Kaiser Permanente is like a big nest that keeps everyone connected and safe from falling through the cracks.
It’s the interconnectivity between all the departments. Our nurses provide care from the heart, not just the brain.
I saw the care we practice here when I first came to work as a medical assistant with an amazing doctor. I also saw it firsthand as a patient myself.
-
Social Share
- Share Celebrating Our Extraordinary Nurses on Pinterest
- Share Celebrating Our Extraordinary Nurses on LinkedIn
- Share Celebrating Our Extraordinary Nurses on Twitter
- Share Celebrating Our Extraordinary Nurses on Facebook
- Print Celebrating Our Extraordinary Nurses
- Email Celebrating Our Extraordinary Nurses

July 16, 2025
A new gold standard in nursing excellence
Woodland Hills Medical Center is our first hospital in Southern California …

April 30, 2025
A history of trailblazing nurses
Nursing pioneers lay the foundation for the future of Kaiser Permanente …

April 30, 2025
Celebrate National Nurses Week with me
Join us in honoring our nurses for their dedication to providing high-quality, …

February 24, 2025
Honoring extraordinary nurses
Our award-winning nurses put patients first and contribute new knowledge …

April 9, 2024
Building partnerships to inspire the next generation
Kaiser Permanente supports education and career opportunities for students …

October 3, 2023
Nursing excellence recognized at Fontana Medical Center
The prestigious Magnet® designation affirms the compassion, dedication, …

August 8, 2023
Nursing excellence: Joining the elite 10% in the nation
Kaiser Permanente Panorama City Medical Center achieves coveted Magnet® …

May 18, 2023
The gold standard of nursing excellence
Kaiser Permanente Baldwin Park Medical Center achieves Magnet status, the …

May 26, 2022
Nurse practitioners: Historical advances in nursing
A doctor shortage in the late 1960s and an innovative partnership helped …

September 28, 2020
A legacy of disruptive innovation
Proceeds from a new book detailing the history of the Kaiser Foundation …
August 26, 2020
Kaiser Permanente’s pioneering nurse-midwives
The 1970s nurse-midwife movement transformed delivery practices.
May 18, 2020
Nurses step up in crises
Kaiser Permanente nurses have been saving lives on the front lines since …

April 30, 2018
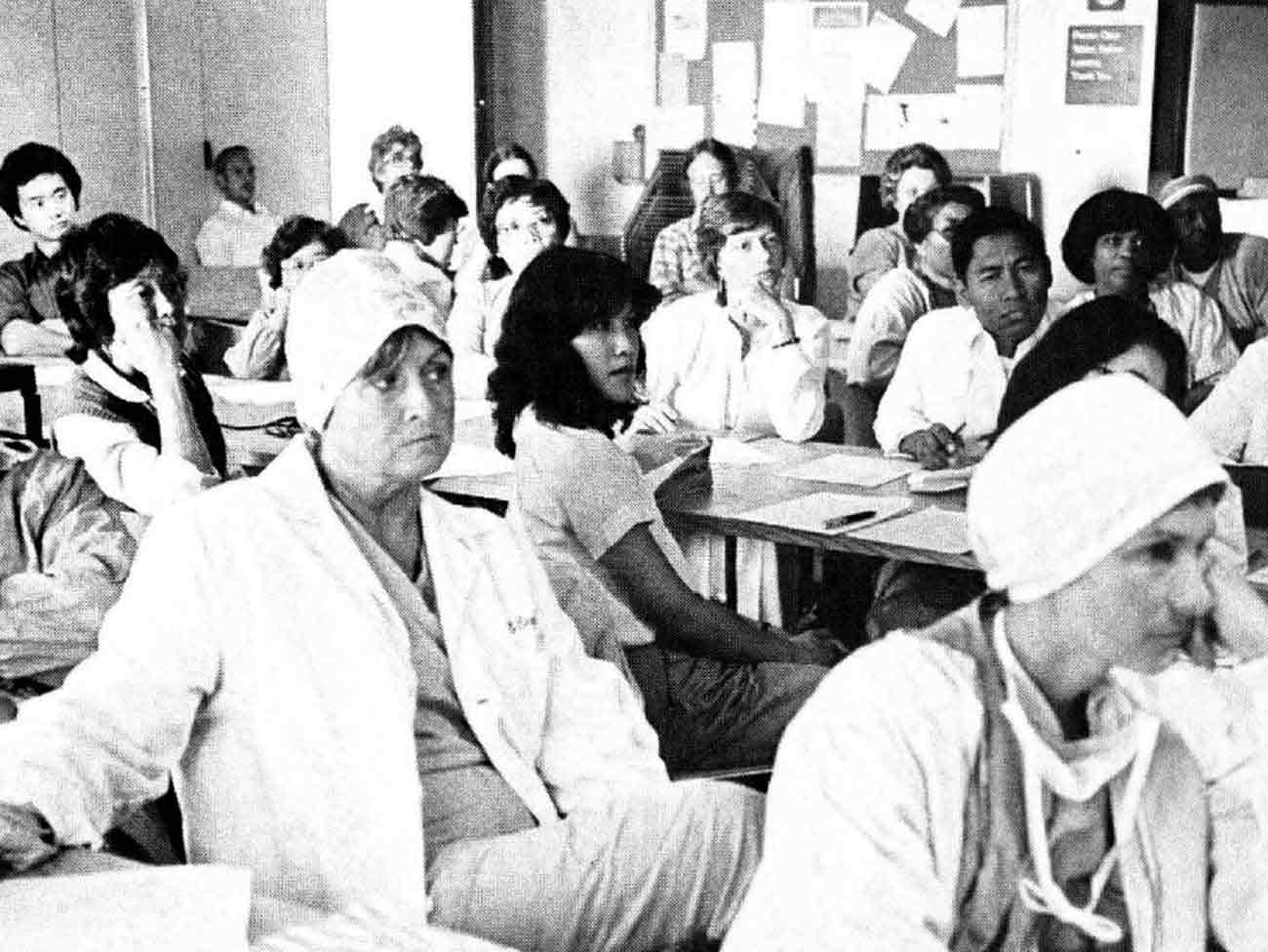
Nursing pioneers leads to a legacy of leadership
Kaiser Foundation School of Nursing students learned a new philosophy emphasizing …

May 4, 2017
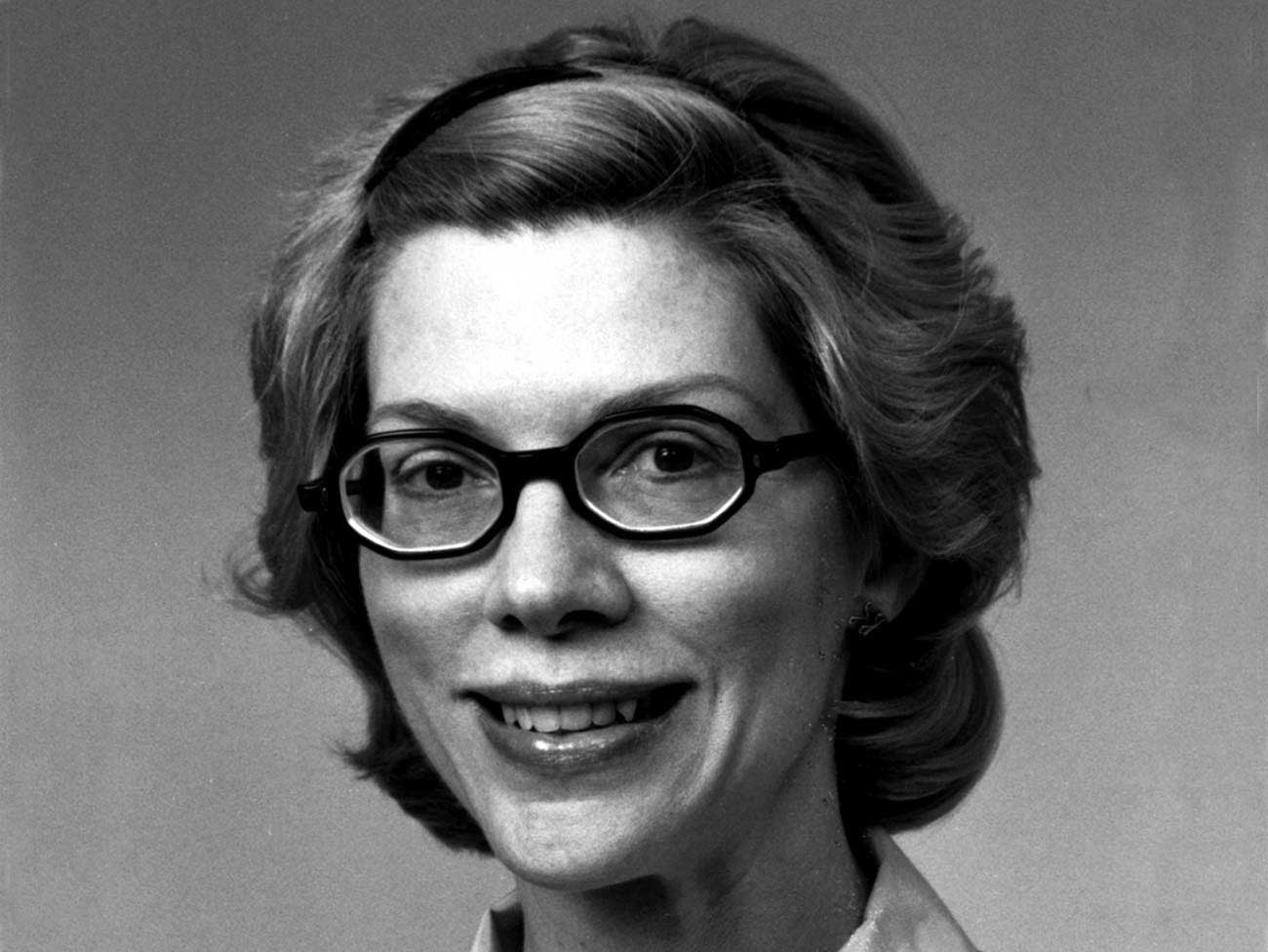
How a Kaiser Permanente nurse transformed health education
Kaiser Permanente's Health Education Research Center and Health Education …

May 5, 2016
Male nursing pioneers
Groundbreaking male students diversify the Kaiser Foundation School of …

July 1, 2015
Sculpture dedicated to Kaiser Nursing School
The Kaiser Foundation School of Nursing sculpture near Kaiser Oakland hospital …

May 6, 2015
Celebrating Betty Runyen — Kaiser Permanente’s ‘founding nurse’
In a desert hospital during the Great Depression, Betty Runyen overcame …

June 20, 2014
Old hospital holds memories of Kaiser Permanente’s past
Rebuilt Oakland Medical Center to open for business.
May 5, 2014
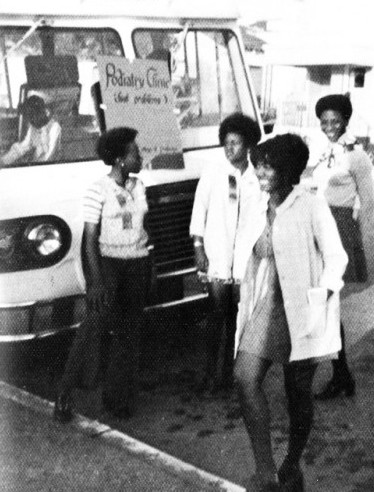
Black nurses get together to forge their own future
California African American nurses organize in early 1970s to address health …

May 1, 2014
Beloved nurse earned place in Kaiser Permanente history
Jessie Cunningham, the first Black nursing supervisor at Oakland Medical …

July 27, 2012
Millie Cutting: physician’s wife makes her own mark
From coordinating community groups to the World War II home front, Millie …
July 1, 2011
Maternity care evolves to embrace family
Shortened in the 1970s led Kaiser Permanente to offer prenatal classes …
June 2, 2011
Kaiser Permanente nursing excellence: 75 years in the making
The founding principles and vision of nursing started in 1933. and paved …

April 30, 2011
Nurses begin quest for professional recognition after World War II
Co-founder Dr. Sidney Garfield makes history by signing the first nurse …

March 20, 2011
Iron nurse Dorothea Daniels had a soft spot for nursing students
The Kaiser Foundation School of Nursing students received effective curriculum …