Collaboration is key to keeping people insured
With the COVID-19 public health emergency ending, states, community organizations, and health plans should partner to help people maintain Medicaid and other coverage.
The COVID-19 pandemic has had a devastating impact since 2020, but there was a bright spot: Thanks to pandemic-era policies that took advantage of Medicaid and extended subsidies under Affordable Care Act coverage, 91 million Americans are now insured, a dramatic increase over 2020.
Now, some of those policies are ending. As a result, millions of people’s Medicaid health coverage eligibility will be reassessed, and there is a significant risk that many people could end up uninsured.
States, policymakers, health plans, local agencies, and community-based nonprofits have an immediate need to work together and take action to make sure people stay covered.
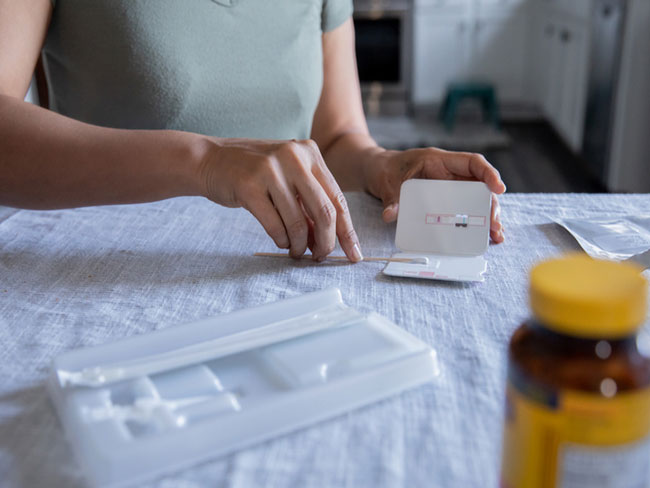
Medicaid and the burden of redetermination
For almost 60 years, Medicaid has provided coverage for people with low incomes and disabilities, including preventive care, mental health services, and more. To prove they remain eligible for benefits, Medicaid recipients must periodically complete the Medicaid renewal process, also known as redetermination or recertification. For many, it can be daunting. Long forms, uneven internet access, changes in address, and language barriers all present challenges.
During the pandemic, lawmakers expanded who was eligible for Medicaid with policies that paused renewals and terminations. With those temporary pandemic policies expiring, a Department of Health and Human Services analysis estimates that about 15 million Medicaid beneficiaries — 1 in 5 — may no longer qualify because they earn too much or haven’t completed the required renewal forms. People with limited English proficiency and people with disabilities may be at the greatest risk of losing coverage, especially in cases where renewal forms aren’t translated into their native language or made easily accessible.
The results could range from a temporary inconvenience to a major disruption of critical health care services. People who lose coverage and remain uninsured often skip necessary care, leading to worse health outcomes and financial distress. They often rely on the emergency room for care, making care management difficult. The results can be fatal.
Keeping people covered
Fortunately, policymakers and health care leaders share the same goal: to help people stay covered. Before the Affordable Care Act, a person ineligible for Medicaid (who didn’t get insurance from an employer) had few options. Today people can get coverage through government-administered marketplaces offering private coverage choices, with subsidies to help ensure individuals and families can afford their insurance premiums.
The challenge for public leaders and health plans is to reach every Medicaid beneficiary to tell them about renewal and educate them about the process. If still eligible, they can remain on Medicaid. If not, coverage through their state or federal marketplace may be the answer.
People no longer eligible for Medicaid may have marketplace options that let them keep their existing health plan and care teams. Therefore, public leaders and health plans also need to educate people about how to remain with their current health plan even if their coverage type changes. Staying with the same plan can mean continuity — keeping your current doctor and other trusted care providers.
Some states plan to automatically enroll people in an exchange plan offered by the same health insurer as their Medicaid plan. In other states people who leave Medicaid could be automatically enrolled in the plan with the lowest premium, even if that plan has a significantly different provider network.
It will be important to make it easy for those people put in a different plan to switch to a plan with the same prior network of providers if they desire.
Permanent policy action needed
States must take full advantage of new outreach opportunities to alert people about Medicaid renewal and their options. Historically, laws have prevented states and health plans from sharing information about beneficiaries and contacting them on personal devices. But temporary policy changes now give states flexibility to partner with health plans to get beneficiaries’ contact information and reach out using calls, text messages, direct mail, and social media.
These policy changes give states an efficient and convenient way to connect people to community resources that can assist them with renewal forms. Lawmakers should make the policies permanent. In today’s world, health plans and states should always be able to contact people via the means each person prefers to alert them about their coverage.
Kaiser Permanente’s approach
Continuity of care for our members and others affected by the Medicaid renewal effort is our highest priority. We are committed to doing all we can to ensure no one goes without coverage.
Because we offer one of the highest-rated Medicaid plans in the country, Kaiser Permanente has developed a national, multi-touch strategy to reach our current Medicaid members. Over the course of 2023, we’re contacting them using mailings, emails, calls, texts, and more. We’re telling them how to navigate the renewal process and the options available if they no longer qualify for Medicaid.
The challenge ahead
Millions of Americans could lose health care coverage in the coming months if we don’t act. But we can work together to reach people in new ways, delivering accessible messages and offering needed guidance. Working together, we can make sure we continue to increase the number of people who have high-quality coverage.