How do physicians know they’re doing the right thing?
Collaborative Kaiser Permanente physicians implemented a new quality program emphasizing the continuous development and update to the standards of care in 1991.
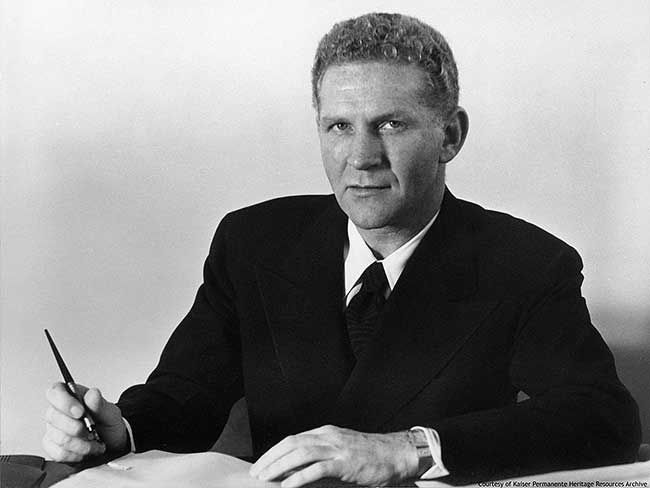
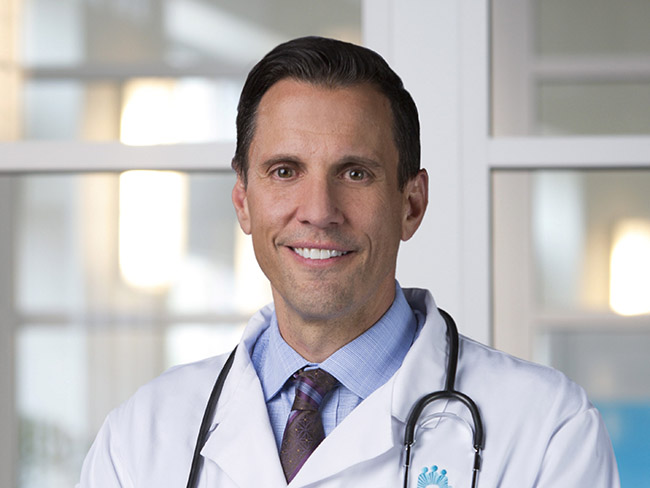
David Lawrence, MD, health plan CEO, a prime mover in the Quality Agenda program launched in 1991. Spectrum photo 1991.

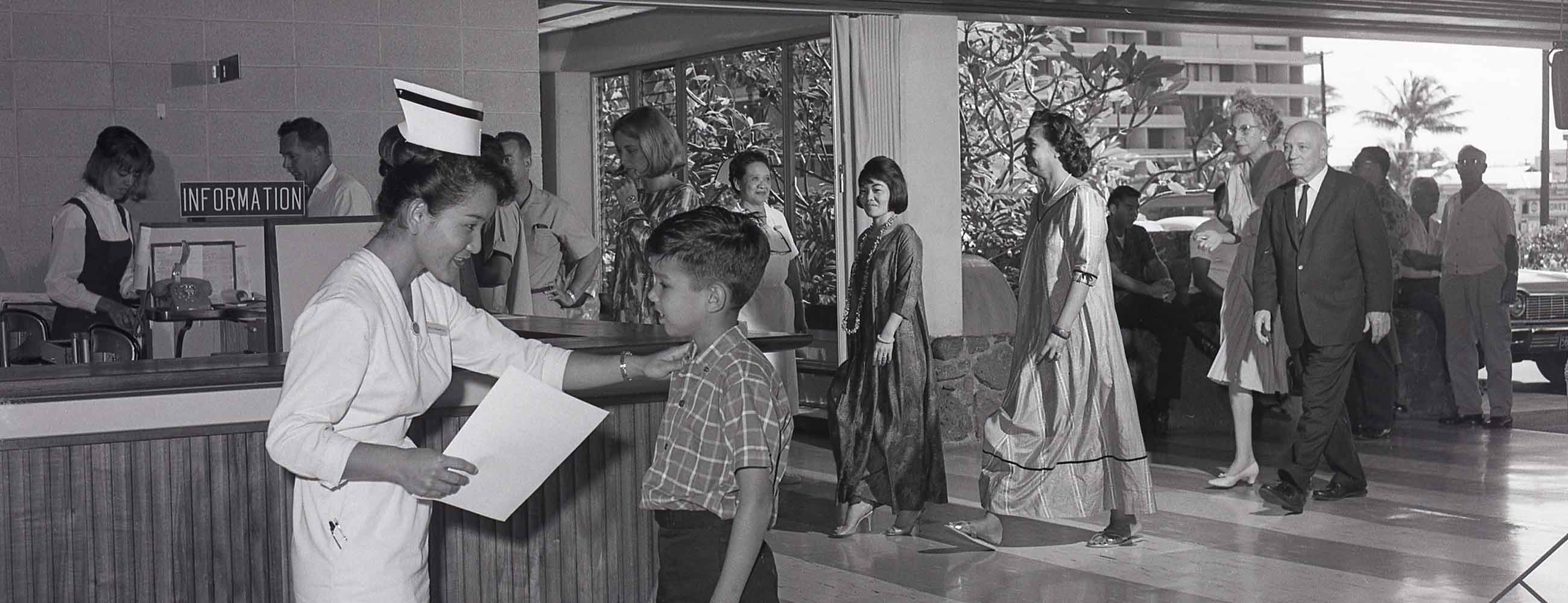
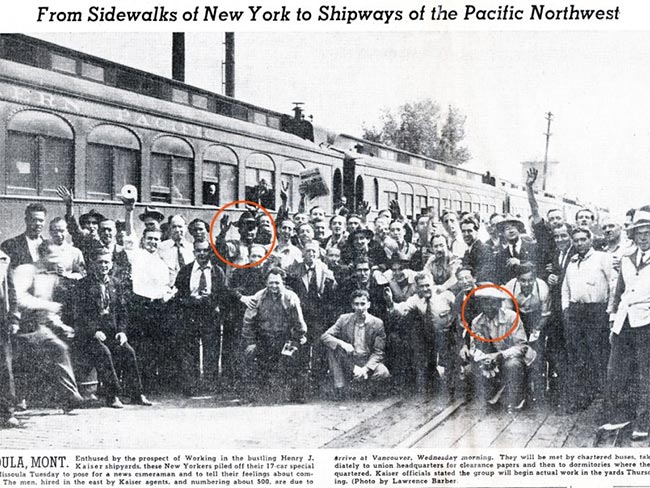
Kaiser Permanente founding physician Sidney Garfield, circa 1933. Garfield’s spirit of innovation and ever-improving health care lives on.
Medical doctors have been plagued for generations with a nagging uncertainty about what treatment is the best for each patient who seeks care. Without scientific proof of the value of treatment, how was he or she to know for sure the care provided would cure and not harm. Tradition and conventional wisdom had to suffice in the absence of research and hard facts. Little was cut and dried.
As medical science advanced in the 20th century, more research offered more knowledge. But as technology raced ahead, it seemed to leave more questions than answers in its wake. Is it worth the risk, worth the expense? How can we predict the outcome?
Enter the quality of care watchdogs of the 1970s, 1980s, and 1990s. The federal government, employers, and consumers were organizing to pressure all health care providers, especially health maintenance organizations, like Kaiser Permanente, to demonstrate high quality.
Kaiser Permanente physicians, who had been exploiting the benefits of practicing in a collaborative and forward-thinking group for 50 years, found themselves at a crossroads. Having grappled with the quality issue already for decades, Permanente physicians took a collective deep breath and again launched into a quest for an effective way to prove Kaiser Permanente's quality of care. This time, they knew they had to take dramatic action.
Quality Agenda gets new energy from medical groups
The first comprehensive initiative was unveiled in 1991 — the Quality Agenda — inspired by Donald Berwick, MD, the Total Quality Management (TQM) proselytizer. Kaiser Permanente leaders adopted TQM and implemented an aggressive new quality program modeled on its principles. This movement launched several programs that emphasized developing and continually updating standards of care in tandem with the National Committee on Quality of Care (NCQA) and other review groups. (See previous blogs posted March 21 and 28.)
But in 1994, Permanente physicians and David Lawrence, CEO, of Kaiser Permanente Health Plan and Hospitals, concluded that the 1991 TQM initiative had not done enough to propel Kaiser Permanente quality efforts forward.
Sharon Conrow, director of Quality Systems, later explained the rationale in a 1999 Permanente Journal article, co-authored with Rob Formanek, MD, the medical director for The Permanente Federation.
“The Boards’ annual reviews continued through the early 1990s and led to continued improvement of the Kaiser Permanente regions’ quality processes and infrastructure,” she wrote. “However, these efforts neither inspired the rapid improvements necessary to meet growing expectations (of consumers and others) nor led to the improvement needed for compliance with NCQA requirements or HEDIS (Health Plan Employer Data and Information Set).
Quality leaders, looking back on these events from 1999, noted that regional quality efforts had been mainly successful over the years, but that the Kaiser Permanente National Health Plan board of directors and Kaiser Permanente physician groups — as a national entity — were ultimately responsible for the quality of care and patient safety, and they had to take the helm. In 1996, Lawrence asked the Permanente medical group directors in all the regions to propose a new approach to quality review.
Medical Directors’ Quality Committee established
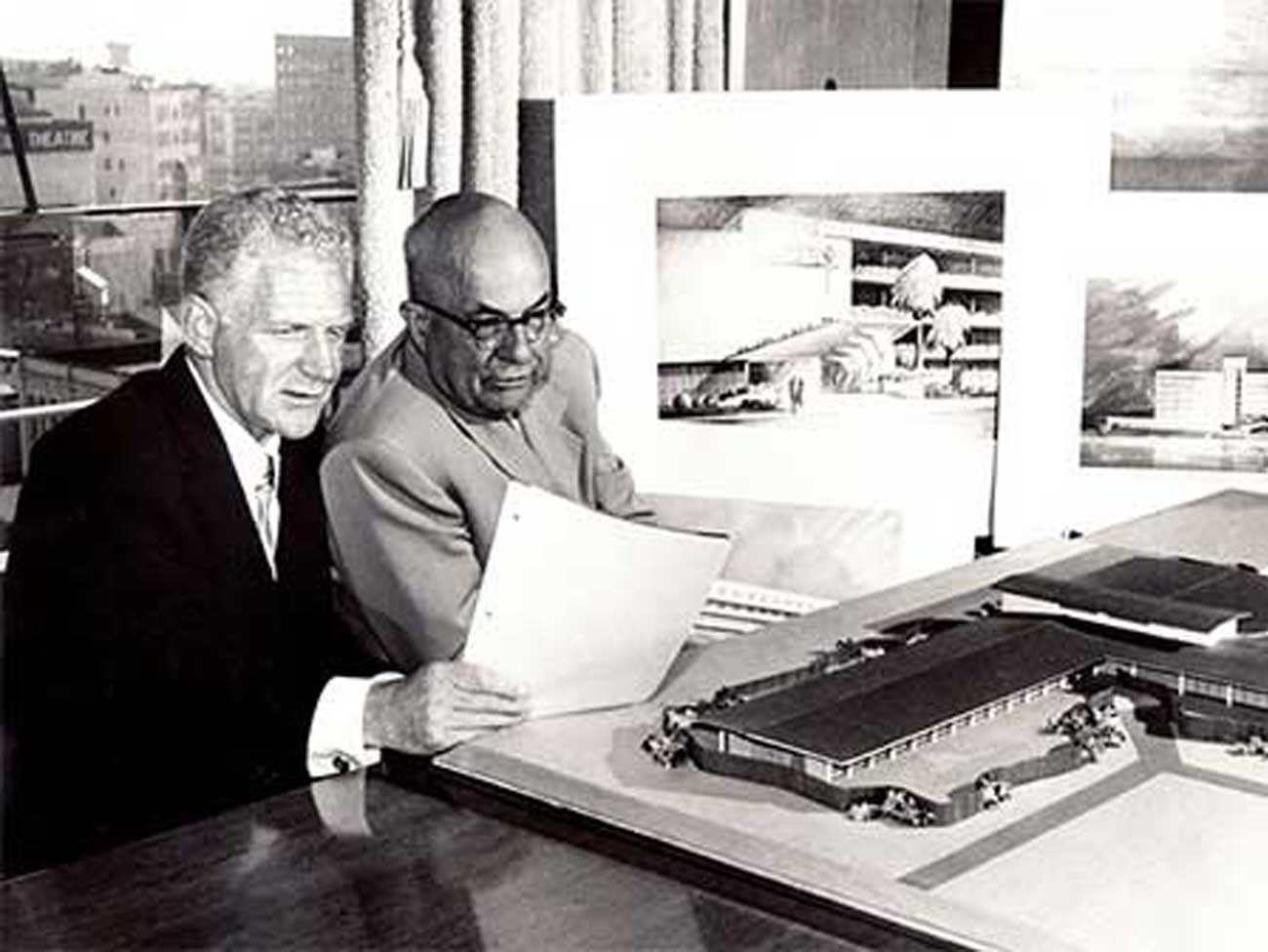
“Quality Initiatives & Outcomes Projects: Firmly Planted: Far Reaching,” Kaiser Permanente report, 1996
The medical groups and health plan and hospital officials set the quality scheme in motion by creating the Medical Directors Quality Committee (MDQC) in 1995. To put additional power behind the initiative, the physician groups formed a strong alliance among all the Kaiser Permanente medical groups. The alliance was initially called the Permanente Medical Group Interregional Service and was renamed in 1997 to The Permanente Federation (TPF) as it’s called today.
In “Quality Initiatives and Outcome Improvement,” an update of the Quality Agenda published in December of 1996, the MDQC and the resultant MDQR (Medical Directors’ Quality Review) were discussed. It was described as a program to “complement and enhance other quality review work processes, such as accreditation by the National Committee for Quality Assurance. The emphasis is on peer-to-peer evaluation and on using the review not just for quality assessment but as a powerful tool for quality improvement across the (Kaiser Permanente health) plans.”
Care Management Institute established to develop clinical guidelines
One of the first charges for the new health plan-medical group partnership (Kaiser Permanente Partnership Group, founded July 1997) was to devise a system to standardize physician performance in all Kaiser Permanente regions. These common practice guidelines, collectively called Permanente Medicine, had to be based on scientific evidence. To accomplish this, in 1997 the partnership established the Care Management Institute (CMI), which develops clinical guidelines based on the strength of available scientific research.
In 2002, departing CEO David Lawrence, MD, told Managed Care magazine: “We’ve agreed that we need to review the scientific evidence and medical evidence in a systematic way and then disseminate it through the entire organization. As a result, a doctor in Atlanta uses the same science and set of evidence and practices with the same understanding of what’s best for the patient as a doctor in Hawaii uses.”
In a 2007 article, Jay Crosson, MD, president of The Permanente Federation for its first 10 years, draws a parallel between Kaiser Permanente physician founder Sidney Garfield’s insistence on constant change and innovation and the quality improvement work the MDQC had done since 1997. “Out of the (national agreement) came not only The Permanente Federation but the Care Management Institute — a jointly managed entity with a mandate to pursue the kind of program-wide quality improvements that Dr. Sidney Garfield envisioned ...”