Can the badly broken prescription drug market be fixed?
Prescription drugs are unaffordable for millions of people. With the right policy solutions, we can get back on the path to affordability.
The high cost of prescription drugs is making them unaffordable for patients.
By Anthony A. Barrueta, Senior Vice President, Government Relations
In a free market, sellers compete on price, and buyers choose the lowest priced good that meets their needs. It’s a fundamental law of economics.
But in the real world, this law sometimes crumbles — especially in America’s prescription drug market.
Drugmakers rarely compete on price. This is one reason why the U.S. spent over $633 billion on prescription drugs last year.
Compared with other high-income countries, the U.S. has the highest per capita prescription drug spending.
How government policies led to higher drug prices
Starting in 1990, a series of policy changes undermined any leverage buyers had to help rein in rising costs.
- Medicaid Drug Rebate Program — Congress introduced the Medicaid Drug Rebate Program in 1990. Under this law, in exchange for having all of their drugs covered, drugmakers agree to pay rebates to state Medicaid programs. Because the law requires that Medicaid receive the “best price,” manufacturers cannot offer deeper discounts to private purchasers. This price floor means Americans with private health insurance (that is, most Americans) pay higher prices for drugs and higher premiums for drug coverage than they otherwise could.
- Health plans covering most drug costs — Over time, health plans have paid for a larger share of the total cost of prescription drugs. Even before Medicare started offering prescription drug coverage in 2006, consumers had become more insulated from the full price of drugs. This helped consumers afford their medications. But patients and their doctors are often unaware of the full price of a drug. They have no reason to seek or choose an equally effective, lower-priced alternative.
- Loopholes in patent laws — When the federal government grants a drugmaker a patent, only the company that holds the patent can make and sell the drug for a period of time. Without competition, these drugmakers can set whatever price they like. Patents are important to stimulate innovation. But there are loopholes. In some cases, drugmakers get patents — and great financial rewards — based on publicly financed drug research. Sometimes they build a complex web of patents. Called patent thickets, these webs make it much harder for competitors to come to market.
This combination of policies has allowed manufacturers to raise prices relentlessly without fear of political or market consequences.
Policy solutions
The broken prescription drug market makes health care unaffordable for millions. But we have some policy options, including:
- Addressing anticompetitive behavior. We can build a fairer patent system. New legislation in Congress addresses patent thickets and more.
- Increasing the use of biosimilars. At Kaiser Permanente, we use the biosimilar versions of drugs whenever possible. They’re equally effective and less expensive. For example, we’ve switched most of our members to the newest biosimilar for Humira, a prescription medication for rheumatoid arthritis and other inflammatory diseases. This saved close to $300 million in 2023 alone.
Humira has a list price of $7,000. By switching members to the biosimilar, we lowered costs for our members and employer groups. Congress should make it easier for doctors to use biosimilars with their patients.
- Focusing on the evidence of a drug’s safety and efficacy. We pay far too much for drugs that don’t improve health outcomes or that show little value over alternative treatments. New policies should strengthen how the Food and Drug Administration approves drugs. This will ensure that available drugs are safe and work well.
- Strengthening Medicare’s ability to negotiate drug prices. Thanks to a law passed in 2022, Medicare can now negotiate the price of a few of the costliest drugs in the US. The drug industry is pushing back aggressively through lawsuits and heavy lobbying. Congress should stand firm and build on this law to protect both Medicare and its beneficiaries into the future.
- Tackling drug shortages. Shortages of specific drugs prevent patients from getting the treatment they need. These shortages also cause rising prices. It’s time our government did more to incentivize companies to make more generic (lower cost) drugs in America. And we need policies that compel drug manufacturers to share more information about their supply pipeline. Then health care systems and providers can identify problems earlier.
The prescription drug market is broken.
It’s time for our lawmakers to have some serious conversations about solutions. Patients deserve access to effective drugs at prices we all can afford.
-
Social Share
- Share Can the Badly Broken Prescription Drug Market Be Fixed? on Pinterest
- Share Can the Badly Broken Prescription Drug Market Be Fixed? on LinkedIn
- Share Can the Badly Broken Prescription Drug Market Be Fixed? on Twitter
- Share Can the Badly Broken Prescription Drug Market Be Fixed? on Facebook
- Print Can the Badly Broken Prescription Drug Market Be Fixed?
- Email Can the Badly Broken Prescription Drug Market Be Fixed?

February 18, 2026
A better approach to preventing chronic conditions
With the right support from our policy leaders, we can help ensure fewer …

January 16, 2026
The importance of childhood vaccinations
Kaiser Permanente continues to recommend the vaccines that have been on …

January 14, 2026
Allegations related to Medicare risk adjustment resolved
The settlement agreement reached with the Department of Justice contains …

December 15, 2025
‘Free’ drug samples aren’t really free
Pharmaceutical marketing hurts patient care and drives up costs. At Kaiser …

December 9, 2025
Buprenorphine saves lives. Why can’t more patients get it?
Policy changes are crucial for better opioid addiction treatment.

December 5, 2025
The importance of hepatitis B vaccination for newborns
Kaiser Permanente will continue to offer the hepatitis B vaccine at birth …

November 19, 2025
Will AI rules leave small hospitals behind?
Policymakers can design regulations that protect patients and work for …

November 5, 2025
Update on mental health program progress
The investments we’ve made over the last several years have resulted in …
November 4, 2025
A best place to work for veterans
As a 2025 top Military Friendly Employer, Kaiser Permanente supports veterans …

October 21, 2025
Health coverage is key to early breast cancer detection
Timely screenings save lives and lower costs, but millions of people miss …

October 15, 2025
Kaiser Permanente shows up strong for the annual plane pull
Championing health equity and teamwork drives Kaiser Permanente’s support …

September 5, 2025
Congress must act to keep health insurance affordable
Enhanced premium tax credits help millions of people afford health insurance. …

August 5, 2025
Pharmaceutical marketing hurts patient care
At Kaiser Permanente, our doctors and pharmacists work together to ensure …

July 22, 2025
Mental health care without borders
When clinicians can practice across state lines, more people can get the …

June 26, 2025
Our commitment to vaccine access
Kaiser Permanente’s statement on vaccine access.

June 17, 2025
We must grow the health care workforce
At Kaiser Permanente, we educate future clinicians and offer programs that …
May 21, 2025
Trust unlocks AI’s potential in health care
Artificial intelligence can improve health care by reducing administrative …

April 21, 2025
Congress must protect Medicaid and insurance tax credits
Medicaid and tax credits for acquiring coverage are essential for patients, …

March 27, 2025
We’re committed to mentorship, mental health, and communities
Kaiser Permanente awarded Elevate Your G.A.M.E. a grant to expand program …

March 25, 2025
AI in health care: 7 principles of responsible use
These guidelines ensure we use artificial intelligence tools that are safe …

March 24, 2025
Our nation's health depends on coverage
Health insurance is key to a strong country — it improves health and boosts …
March 17, 2025
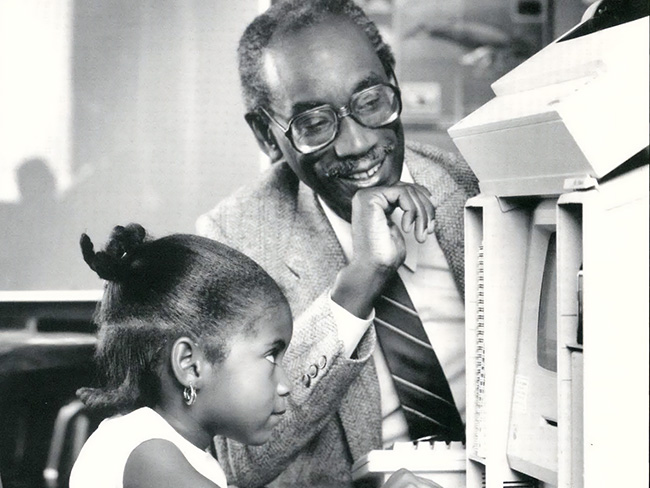
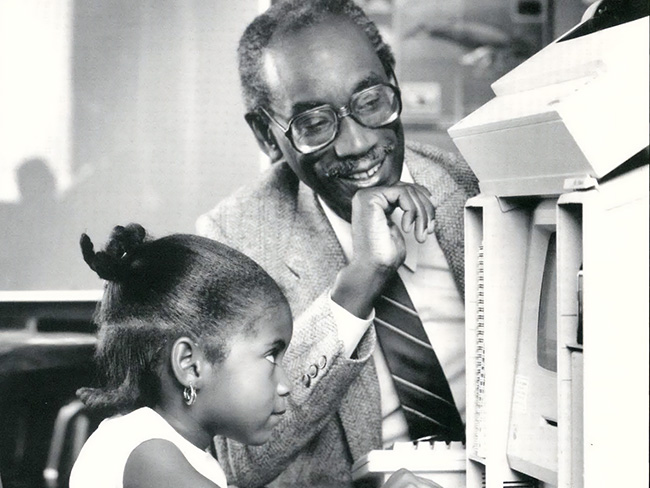
Remembering Bill Coggins and his lasting legacy
The founder of the Kaiser Permanente Watts Counseling and Learning Center …

February 20, 2025
Our nation’s health suffers if Congress cuts Medicaid
Reducing Medicaid funding will lead to worse health outcomes, overburden …

January 15, 2025
Why the U.S. needs more community health workers
With the right strategies and public policies, we can strengthen our nation’s …

January 10, 2025
Kaiser Permanente and UFCW Local 7
Read our statement.

December 26, 2024
Linking isolated communities to care
A collaborative partnership, powered by trusted nonprofit partners, brings …

December 10, 2024
Accelerating growth in the mental health care workforce
Actions policymakers can take to grow and diversify the mental health care …

November 11, 2024
Health care coverage now accessible to uninsured people
Indigenous farmworkers may qualify for new Kaiser Permanente coverage.

November 11, 2024
Medicare telehealth flexibilities should be here to stay
We urge Congress to extend policies that have improved access to care and …

October 15, 2024
Our dedication to fostering well-being and equity
The 2023 Kaiser Permanente Southern California Community Health County …

September 16, 2024
Voting affects the health of our communities
In honor of National Voter Registration Day, we encourage everyone who …

July 22, 2024
Our nation’s health depends on well-funded research
Advanced medical science improves patient outcomes. We urge lawmakers to …

July 16, 2024
Teacher residency program improves retention and diversity
A $1.5 million Kaiser Permanente grant addresses Colorado teacher shortage …

June 19, 2024
Investments in Black community promote total health for all
Funding from Kaiser Permanente in Washington helps to promote mental health, …

April 12, 2024
It’s time to address America’s Black maternal health crisis
Health care leaders and policymakers should each play their part to help …

March 19, 2024
Fostering responsible AI in health care
With the right policies and partnerships, artificial intelligence can lead …

March 18, 2024
Program helps member prioritize her health
Medical Financial Assistance program supports access to health care.
March 6, 2024
Former employee honored for supporting South LA families
Bill Coggins, who founded the Kaiser Permanente Watts Counseling and Learning …
March 4, 2024
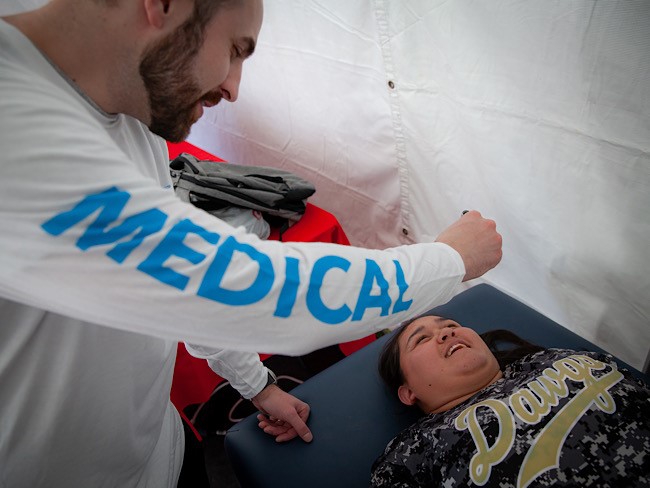
Taking care of Special Olympics athletes
Kaiser Permanente physicians and medical students provide medical exams …

February 12, 2024
Proposition 1 would bolster mental health care in California
Kaiser Permanente supports the ballot measure to expand and improve mental …

February 2, 2024
Expanding medical, social, and educational services in Watts
Kaiser Permanente opens medical offices and a new home for the Watts Counseling …

January 31, 2024
Prioritizing policies for health and well-being in Colorado
CityHealth’s 2023 Annual Policy Assessment awards cities for their policies …

January 22, 2024
Solutions for strengthening the mental health care workforce
Better public policies can help address the challenges. We encourage policymakers …

December 20, 2023
Funding solutions to end gun violence
Researchers and organizations are exploring inventive ways to reduce gun …

December 20, 2023
Championing inclusivity at the Fall Games
Kaiser Permanente celebrates inclusion at Special Olympics Southern California …

December 15, 2023
Climate change is already affecting our health
The health care industry is responsible for 8% to 10% of harmful emissions …

December 7, 2023
Safe, secure housing is a must for health
We offer housing-related legal help to prevent evictions and remove barriers …

December 6, 2023
Solid foundation: How construction careers support health
Steady employment can improve a person's health and well-being. Our new …

November 13, 2023
Congress must act to address drug shortages
Kaiser Permanente is working to address drug shortages and support policies …

November 9, 2023
New 4-year agreement ratified
National agreement between Kaiser Permanente and the Coalition will help …

November 1, 2023
Meet our 2023 to 2024 public health fellows
To help develop talented, diverse community leaders, Kaiser Permanente …

October 12, 2023
Our commitment to transforming mental health care in California
Kaiser Permanente and the California Department of Managed Health Care …

September 8, 2023
Regulated waste settlement in California
We are committed to the well-being of the environment and protecting the …

September 6, 2023
Advancing mental health crisis care through public policy
Organizations that provide public mental health crisis services must work …

August 15, 2023
'Hot-spot' strategy gets more Californians vaccinated
A new location-based vaccine strategy by Kaiser Permanente was successful …

August 10, 2023
Highlighting our community health work in Southern California
The Kaiser Permanente Southern California 2022 Community Health Snapshot …

August 2, 2023
Social health resources are just a click or call away
The Kaiser Permanente Community Support Hub can help members find community …

July 26, 2023
Kaiser Permanente hiring 10,000 new staff for Coalition jobs
More than 6,500 of these union-represented positions have already been …

July 11, 2023
Our prescription for safe, effective, more affordable drugs
Our approaches ensure effectiveness and safety, and drive cost savings. …

June 30, 2023
Our response to Supreme Court ruling on LGBTQIA+ protections
Kaiser Permanente addresses the Supreme Court decision on LGBTQIA+ protections …

June 29, 2023
Our response to Supreme Court's ruling on affirmative action
Kaiser Permanente addresses the Supreme Court decision on affirmative action …

June 29, 2023
Special Olympics athletes go for the gold
Kaiser Permanente celebrated its sixth year as official health partner …

June 14, 2023
Honored for commitment to people with disabilities
The Achievable Foundation recognized Kaiser Permanente for its work to …

June 7, 2023
Engaging businesses for action on climate and health equity
New climate collaborative with BSR announced at joint Kaiser Permanente …

June 1, 2023
Policy recommendations from a mental health therapist in training
Changing my career and becoming a therapist revealed ways our country can …

May 22, 2023
Investing and partnering to build healthier communities
Kaiser Permanente supports Asian Americans Advancing Justice to promote …

May 10, 2023
A workplace for all
We are building inclusive work and care environments where everyone feels …

May 10, 2023
Health equity, inclusion, and belonging
We strive for fairness, respect, and inclusion for all.

May 2, 2023
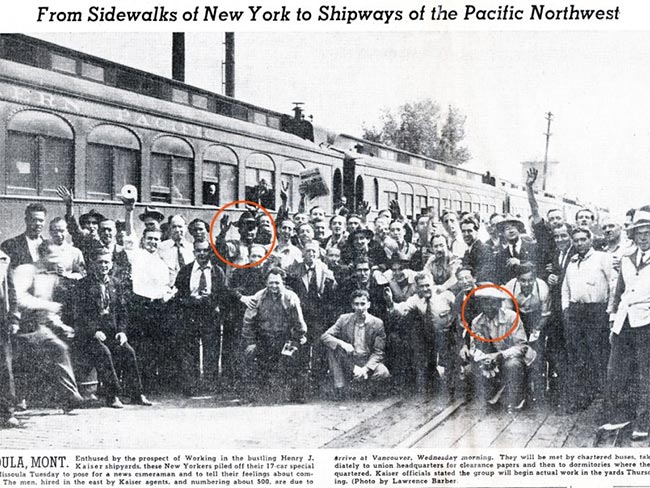
Women lead an industrial revolution at the Kaiser Shipyards
Early women workers at the Kaiser shipyards diversified home front World …

April 27, 2023
Inspiring students to pursue health care careers
Kaiser Permanente is confronting future health care staffing challenges …

April 25, 2023
Hannah Peters, MD, provides essential care to ‘Rosies’
When thousands of women industrial workers, often called “Rosies,” joined …

April 11, 2023
Collaboration is key to keeping people insured
With the COVID-19 public health emergency ending, states, community organizations, …

April 5, 2023
Housing help brings stability to patients’ lives
With medical-legal partnerships, we’re helping prevent evictions. Patients …

April 3, 2023
Hospital patients who are homeless connected to housing
A Kaiser Permanente program connects patients experiencing homelessness …

March 29, 2023
Supporting a safer future with public health
We’re partnering on 3 initiatives to strengthen public health in the United …

February 17, 2023
Good health starts in our communities: 2022 by the numbers
Kaiser Permanente supports total health in our communities in partnership …

January 17, 2023
Lawmakers must act to boost telehealth and digital equity
Making key pandemic-era telehealth policies permanent and ensuring more …

December 5, 2022
Want to lower drug prices? Reform the U.S. patent system
Pharmaceutical manufacturers that exploit the current system drive up …

November 14, 2022
It’s time to rethink health care quality measurement
To meaningfully improve health equity, we must shift our focus to outcomes …

November 11, 2022
High-quality, equitable care
We believe everyone has a right to good health.
November 11, 2022
Early leaders in equity and inclusion
Explore Kaiser Permanente’s commitment to equitable, culturally responsive …

November 8, 2022
Protecting access to medical care for legal immigrants
A statement of support from Kaiser Permanente chair and CEO Greg A. Adams …

October 21, 2022
Kaiser Permanente therapists ratify new contract
New 4-year agreement with NUHW will enable greater collaboration aimed …

August 16, 2022
Our support for the Inflation Reduction Act
A statement from chair and chief executive Greg A. Adams on the importance …

May 2, 2022
How to transform mental health care: Follow the research
We applaud President Biden and Congress as they begin to set policies that …

March 22, 2022
NUHW psych-social employees ratify agreement
The agreement between Kaiser Permanente and the NUHW in Southern California …

March 22, 2022
Our commitment to equity and our LGBTQIA+ communities
A statement from chair and chief executive officer Greg A. Adams.

February 21, 2022
A best place to work for LGBTQ+ equality
Human Rights Campaign Foundation gives Kaiser Permanente another perfect …
February 14, 2022
Health care scholarships available
Kaiser Permanente in Hawaii to provide up to $100,000 in scholarships to …

October 12, 2021
Beyond advocacy: Requiring vaccination to stop COVID-19
Kaiser Permanente and other leading companies are mandating COVID-19 shots …

August 25, 2021
Kaiser Permanente’s history of nondiscrimination
Our principles of diversity and our inclusive care began during World War …

July 7, 2021
Achieving health equity
Equal medical care is not enough to end disparities in health outcomes.
June 2, 2021
Path to employment: Black workers in Kaiser shipyards
Kaiser Permanente, Henry J. Kaiser’s sole remaining institutional legacy, …

April 27, 2021
Health data privacy
Protecting our members’ personal health information

April 23, 2021
Medicaid
Delivering high-quality Medicaid coverage and services

April 27, 2020
Health care reform
Affordable, accessible health care and coverage

March 4, 2020
Our impact
How Kaiser Permanente strengthens communities and advances public policies …

March 1, 2020
Prescription drug pricing
Bringing down the high cost of medication

February 29, 2020
California
