A conversation about pregnancy and women’s heart health
New research shows blood pressure patterns early in pregnancy can identify the risk of later pregnancy-related high blood pressure conditions.
Doctors can use information about pregnancy-related complications to assess your overall risk of future cardiovascular disease and help you take steps to reduce that risk.
Heart disease is the leading cause of death for women in the United States. One of the leading risk factors for heart disease — high blood pressure — usually has no symptoms, so many women don’t know they have it. And sometimes, it can develop during pregnancy, putting both mother and child at risk.
Erica Gunderson, PhD, a Kaiser Permanente senior research scientist and epidemiologist, is bringing awareness to how pregnancy may affect women’s heart health.
Gunderson’s research showed that blood pressure patterns seen during the first 20 weeks of pregnancy can identify patients who are most likely to develop high blood pressure complications — known as preeclampsia and pregnancy-related hypertension later in their pregnancies. Preeclampsia, which is often signaled by high blood pressure and too much protein in urine, can affect other organs such as the kidney and liver.
Gunderson discusses her research and how women can use this information to better understand their risk of heart disease.
Which heart disease risk factors should women watch for?
Although there are many risk factors — such as high blood pressure, diabetes, obesity, smoking, and lifestyle behaviors — that men and women share, unhealthy pregnancy outcomes such as pregnancy-related hypertension and preeclampsia are unique to women.
In my recent study, we found that blood pressure measurements taken in the first half of pregnancy can identify patterns that signal a higher risk of developing hypertensive disorders during pregnancy beyond clinical factors, such as a first birth and high body weight. If doctors are aware of these patterns they may be able to identify these higher-risk patients earlier, and may be able to help them avoid pregnancy complications from hypertension.
Hypertension during pregnancy can have implications for women’s heart health beyond pregnancy, too. Previous studies have shown that women who experienced complications related to high blood pressure during pregnancy have an increased risk for developing cardiovascular disease later in life.
What did your research find about racial disparities among pregnant women with high blood pressure?
Research shows that Black and Hispanic women are most likely to experience heart disease. Black women are also significantly more likely to have high blood pressure before pregnancy and develop high blood pressure during pregnancy.
Consistent with previous research, my study of women who did not have high blood pressure before they became pregnant found that being Black or Hispanic was associated with a higher risk of developing hypertensive disorders during pregnancy. Other factors that increased risk during pregnancy were being younger, overweight, or obese before pregnancy, or not giving birth before.
Researchers are still working to understand the reasons why Black and Hispanic women have a higher risk of hypertensive disorders during pregnancy. Higher rates of hypertension before pregnancy, having more elevated blood pressure patterns during early pregnancy, and social drivers of health such as socioeconomic status and access to healthy food and health care, may play a role.
What can women do to better understand their risk for heart disease?
It’s important to know your individual risk factors for heart disease — such as your own medical history and family history of diabetes, high blood pressure, or heart disease, as well as lifestyle factors such as diet, physical activity, and sleep habits.
Our research shows there’s also value in talking to your primary care physician about risk factors before pregnancy, and about any pregnancy-related complications you may have experienced. Doctors can use that information to assess your overall risk of future cardiovascular disease and help high-risk patients take steps to reduce that risk.
Finally, continue to see your primary care physician regularly and monitor your blood pressure consistently if recommended by your doctor.
Learn about ways you can reduce your risk for heart attack and stroke.
AHA Honors Dr. Gunderson
Erica Gunderson, PhD, was honored with the American Heart Association’s 2022 Research Goes Red Award for best scientific publication on cardiovascular disease and stroke in women. Her study is the largest and most diverse study of its kind, including close to 175,000 Kaiser Permanente patients in Northern California.
-
Social Share
- Share A Conversation About Pregnancy and Women's Health on Pinterest
- Share A Conversation About Pregnancy and Women's Health on LinkedIn
- Share A Conversation About Pregnancy and Women's Health on Twitter
- Share A Conversation About Pregnancy and Women's Health on Facebook
- Print A Conversation About Pregnancy and Women's Health
- Email A Conversation About Pregnancy and Women's Health

May 7, 2025
How to cope with anxiety after childbirth
As a new mother, Cherissa Ong was overwhelmed by stress. A mental health …

May 6, 2025
Best maternity hospitals: We have 29 of them
Our high-quality, compassionate care landed us on Newsweek’s 2025 list …

April 25, 2025
Treating the heart and lungs together for a rare disease
With her medical teams working together, Sirina Hazeem is getting her life …

March 27, 2025
We’re committed to mentorship, mental health, and communities
Kaiser Permanente awarded Elevate Your G.A.M.E. a grant to expand program …

March 25, 2025
AI in health care: 7 principles of responsible use
These guidelines ensure we use artificial intelligence tools that are safe …
March 17, 2025
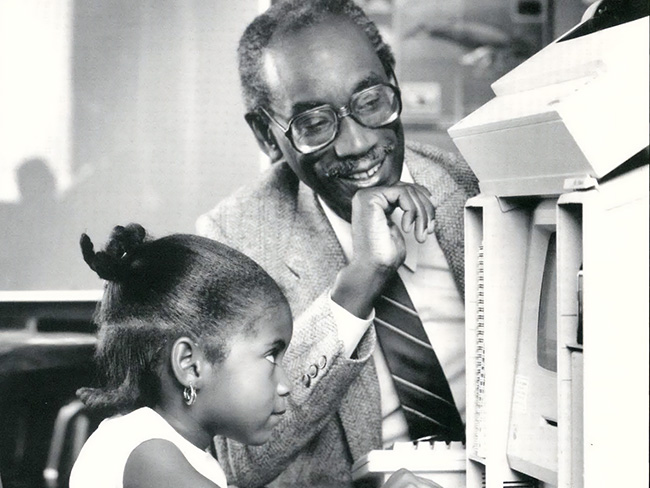
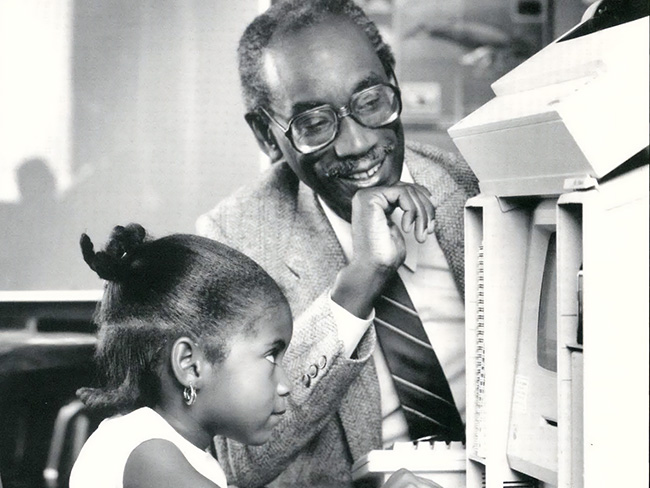
Remembering Bill Coggins and his lasting legacy
The founder of the Kaiser Permanente Watts Counseling and Learning Center …

March 7, 2025
High blood pressure during pregnancy is on the rise
The keys to preventing cardiovascular conditions during pregnancy are knowing …

February 27, 2025
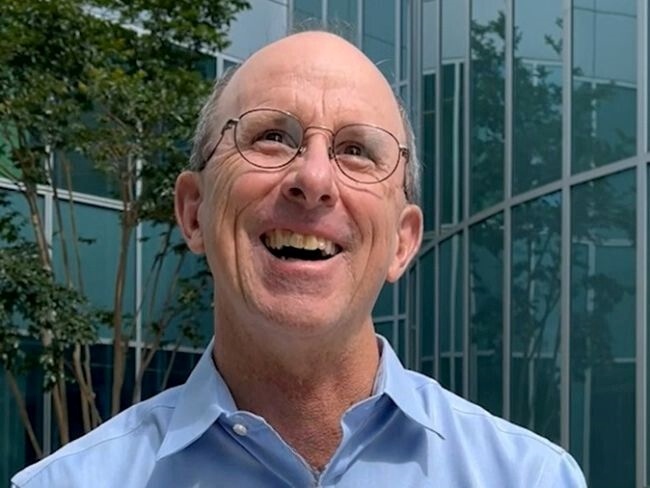
‘The heart attack that saved my life’
A sudden heart attack led Mark Twichel to seek care at Kaiser Permanente …

February 26, 2025
Colon cancer: Do you need to be screened?
If you’re age 45 or older, getting checked regularly for colorectal cancer …

February 21, 2025
Broken heart syndrome: What to know
NPR

February 18, 2025
I just need a chance
Billy Cardosi spent his life putting his family and job first. Then a heart-rela …

February 3, 2025
From a routine appointment to a cardiac crisis
An irregular heartbeat revealed that Enrique Medina had a serious heart …

January 29, 2025
A happy heart is a healthy heart
A cardiologist offers tips to help you improve your health and prevent …

January 24, 2025
Is one drink a day OK? Here’s what to consider
NPR

January 15, 2025
After surgery, home was where his heart was
Virtual cardiac rehabilitation offers Mike Erskine a convenient, safe way …

January 13, 2025
How to prevent cervical cancer
Cervical cancer is highly preventable. HPV vaccination and regular screenings …

December 26, 2024
Linking isolated communities to care
A collaborative partnership, powered by trusted nonprofit partners, brings …

November 11, 2024
Medicare telehealth flexibilities should be here to stay
We urge Congress to extend policies that have improved access to care and …

November 11, 2024
Health care coverage now accessible to uninsured people
Indigenous farmworkers may qualify for new Kaiser Permanente coverage.
November 6, 2024
A best place to work for veterans
As a 2024 top Military Friendly Employer, Kaiser Permanente supports veterans …

October 29, 2024
How poor sleep can hurt your heart
An interview with Kaiser Permanente sleep expert Clarisse Glen, MD, sheds …
October 29, 2024
That’s not tennis elbow
A Kaiser Permanente physician thought he pinched a nerve during a tennis …

October 23, 2024
Doomscrolling? It may affect your heart.
Endless bad news is just one fingertip away online. One Kaiser Permanente …

October 15, 2024
Our dedication to fostering well-being and equity
The 2023 Kaiser Permanente Southern California Community Health County …

October 1, 2024
Screening for breast cancer: Mammogram guidelines
A Kaiser Permanente radiologist answers commonly asked questions.

September 16, 2024
Voting affects the health of our communities
In honor of National Voter Registration Day, we encourage everyone who …

September 6, 2024
Navigating a world turned upside down after heart failure
After a life-threatening series of heart attacks at age 57, Bunnell Fockler …

August 29, 2024
After Stage 4 ovarian cancer, she’s still going strong
Donna Budway received prompt surgery followed by chemotherapy. She credits …

August 15, 2024
Back home one day after heart surgery
Ed Dalmasso needed an aortic valve replacement. His care team provided …

July 16, 2024
Teacher residency program improves retention and diversity
A $1.5 million Kaiser Permanente grant addresses Colorado teacher shortage …

July 11, 2024
Expecting parents find community and support in group visits
Maureen McLoughlin’s experience with care in a group setting gave her the …

July 10, 2024
We help members lower their risk of heart attacks and strokes
A Southern California program, powered by our connected care model, is …

July 2, 2024
Best maternity hospitals: We have 29 of them
Our safe, high-quality, compassionate care landed us on Newsweek’s America’s …

June 25, 2024
Prompt postpartum care saves a baby’s life
When a newborn was diagnosed with meningitis, a life-threatening infection …

June 19, 2024
Investments in Black community promote total health for all
Funding from Kaiser Permanente in Washington helps to promote mental health, …

June 17, 2024
That’s a lot of babies!
Delivering multiple babies is difficult, but Kaiser Permanente care teams …

May 7, 2024
Can the badly broken prescription drug market be fixed?
Prescription drugs are unaffordable for millions of people. With the right …

April 12, 2024
It’s time to address America’s Black maternal health crisis
Health care leaders and policymakers should each play their part to help …

April 10, 2024
For a new mom, talking about her worries helped her heal
One in 5 people experience depression, anxiety, or other mental health …

April 8, 2024
Reducing inequity with fruits and vegetables
Black Americans experience worse health outcomes compared to other populations. …

March 29, 2024
Faster recovery: From cardiac scare to exploring Italy
Virtual cardiac rehab helped Mike Kelly heal at home after a life-threatening …

March 18, 2024
Program helps member prioritize her health
Medical Financial Assistance program supports access to health care.

March 14, 2024
Healthy kidneys support overall good health
Kaiser Permanente excels in preventing, detecting, and treating kidney …

March 14, 2024
Midwife offers personal care for mom facing complications
For Sam Beeson, having a midwife at her side during her pregnancy helped …

March 12, 2024
In-home recovery restores harmony to life
Colorado musician back with the band thanks to new virtual cardiac rehab …
March 6, 2024
Former employee honored for supporting South LA families
Bill Coggins, who founded the Kaiser Permanente Watts Counseling and Learning …
March 4, 2024
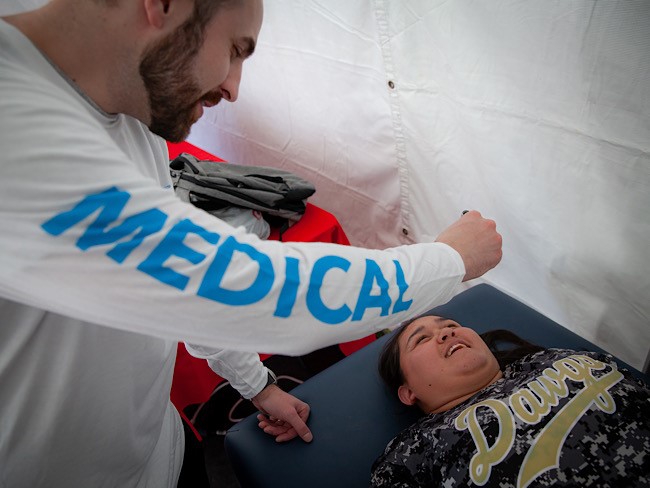
Taking care of Special Olympics athletes
Kaiser Permanente physicians and medical students provide medical exams …
February 22, 2024
The journey of a lifetime
Care teams at Kaiser Permanente Fontana Medical Center helped Phillip Crawford …

February 21, 2024
Recovering at home after a double mastectomy
Innovative surgical recovery program helps breast cancer patients safely …

February 2, 2024
Expanding medical, social, and educational services in Watts
Kaiser Permanente opens medical offices and a new home for the Watts Counseling …

February 1, 2024
Take a break from cannabis while expecting, study suggests
Research shows that marijuana use during pregnancy increases health risks …

January 26, 2024
Retiree back in the swing of things after heart procedure
Tookie Gentilcore returns to enjoying life thanks to a quick, safe method …

January 17, 2024
How diabetes can affect your heart
People with diabetes are more likely to have heart disease.

January 10, 2024
‘You don’t know unless you ask them’
Kaiser Permanente’s Patient Advisory Councils help us create exceptional …

December 20, 2023
Championing inclusivity at the Fall Games
Kaiser Permanente celebrates inclusion at Special Olympics Southern California …

December 19, 2023
Life-changing care for patients who experience strokes
In Oregon, our stroke teams are providing patients with industry-leading …

December 15, 2023
Family-centered care, through pregnancy and beyond
Members experiencing a low risk pregnancy have the option of having their …

December 7, 2023
Safe, secure housing is a must for health
We offer housing-related legal help to prevent evictions and remove barriers …

December 6, 2023
Video prenatal visits are a boon for a busy working mom
A new care option offers a mix of in-person and virtual visits, supported …

December 6, 2023
Solid foundation: How construction careers support health
Steady employment can improve a person's health and well-being. Our new …

November 17, 2023
Expert advice on keeping your heart healthy
Dr. Yong Shin shares how people with heart disease can live longer, while …

November 16, 2023
Providing a bridge to heart transplant
The use of a ventricular assist device implant gives one Oregon woman the …

November 15, 2023
Care at home: Giving patients what they want
Our Advanced Care at Home program provides high-quality, safe care in familiar, …

November 13, 2023
Take a deep breath (we can help with that)
It’s never too late to quit smoking. At Kaiser Permanente, we can help …

November 1, 2023
Meet our 2023 to 2024 public health fellows
To help develop talented, diverse community leaders, Kaiser Permanente …

October 25, 2023
Critical care and support for our youngest patients
In Oregon, specialists and parents come together to design a specialized …

October 25, 2023
Breast cancer during pregnancy: Caring for mom and baby
A team of specialists treats an expecting mother’s cancer while keeping …

October 23, 2023
A renewed sense of purpose after surviving breast cancer
Joy Short, a Kaiser Permanente member and employee, turned her breast cancer …

October 11, 2023
Expanded gun violence prevention efforts
The next phase for the Kaiser Permanente Center for Gun Violence Research …

September 20, 2023
Healing after a heart attack
For years, serious heart attacks meant hours of weekly appointments. Now, …

August 29, 2023
Preventing overdoses starts with education
Risk factors are not always associated with addiction or substance abuse. …

August 18, 2023
Protect your heart when temperatures soar
Excessive heat and pollution can increase your risk of experiencing dangerous …

August 17, 2023
Beyond clinic walls: Research supporting healthy communities
Stories in the Department of Research & Evaluation 2022 Annual Report demonstrat …

August 16, 2023
Cervical cancer screening: Exploring the at-home HPV test
Kaiser Permanente is at the forefront of cervical cancer research. Find …

August 15, 2023
'Hot-spot' strategy gets more Californians vaccinated
A new location-based vaccine strategy by Kaiser Permanente was successful …

August 15, 2023
As temperatures rise, so does the risk of heart problems
A Kaiser Permanente cardiologist shares advice on how to stay safe, what …

August 10, 2023
Highlighting our community health work in Southern California
The Kaiser Permanente Southern California 2022 Community Health Snapshot …

August 2, 2023
Social health resources are just a click or call away
The Kaiser Permanente Community Support Hub can help members find community …

July 27, 2023
Courageously facing hereditary breast cancer
Fay Gordon's breast cancer was caught in the early stages thanks to genetic …

July 26, 2023
Can you get chemotherapy while pregnant?
Chemotherapy can be an option during pregnancy. Find out how Kaiser Permanente …

July 14, 2023
Breast reconstruction surgery after cancer
A Kaiser Permanente plastic surgeon explains breast reconstruction options …

July 11, 2023
We deliver excellence for parents and babies
Our members are more likely to feed their babies breast milk. And they’re …

June 30, 2023
Our response to Supreme Court ruling on LGBTQIA+ protections
Kaiser Permanente addresses the Supreme Court decision on LGBTQIA+ protections …

June 29, 2023
Our response to Supreme Court's ruling on affirmative action
Kaiser Permanente addresses the Supreme Court decision on affirmative action …

June 29, 2023
Special Olympics athletes go for the gold
Kaiser Permanente celebrated its sixth year as official health partner …

June 27, 2023
Men: It’s time to prioritize preventive care
It’s important to be proactive about your health by scheduling regular …

June 21, 2023
And that’s why they call postpartum the blues
Take time to adjust to a new baby and lifestyle changes — and reach out …

June 14, 2023
5 easy ways to reduce heart disease risk
A reminder that men and women can assert control over risk factors that …

June 14, 2023
Living with stage 4 breast cancer
Thanks to personalized care from a team of skilled doctors, Christina McAmis …

June 14, 2023
Honored for commitment to people with disabilities
The Achievable Foundation recognized Kaiser Permanente for its work to …

June 7, 2023
Engaging businesses for action on climate and health equity
New climate collaborative with BSR announced at joint Kaiser Permanente …

May 25, 2023
Grateful for the gift of speech
After experiencing a stroke, K-9 handler Lameka Bell regained near-total …

May 22, 2023
Investing and partnering to build healthier communities
Kaiser Permanente supports Asian Americans Advancing Justice to promote …

May 10, 2023
A workplace for all
We value and respect employees and physicians of all backgrounds, identities, …

May 10, 2023
Equity, inclusion, and diversity
We strive for equity and inclusion for all.

May 2, 2023
Women lead an industrial revolution at the Kaiser Shipyards
Early women workers at the Kaiser shipyards diversified home front World …

April 27, 2023
Inspiring students to pursue health care careers
Kaiser Permanente is confronting future health care staffing challenges …

April 25, 2023
Hannah Peters, MD, provides essential care to ‘Rosies’
When thousands of women industrial workers, often called “Rosies,” joined …

April 14, 2023
The importance of screening for gestational diabetes
Gestational diabetes poses a significant risk to women of color, particularly …

April 12, 2023
Having her ‘rainbow baby’ after a high-risk pregnancy
Remote perinatal monitoring and frequent in-person appointments helped …