Recovering at home after a double mastectomy
Innovative surgical recovery program helps breast cancer patients safely recover at home after a mastectomy. Learn how Kaiser Permanente supports home care.
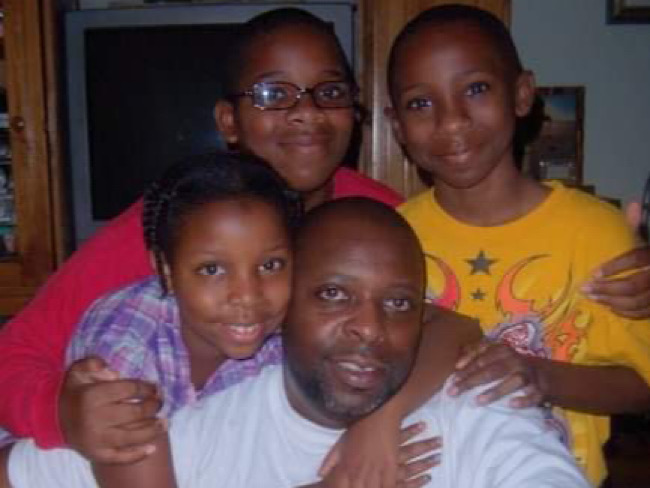
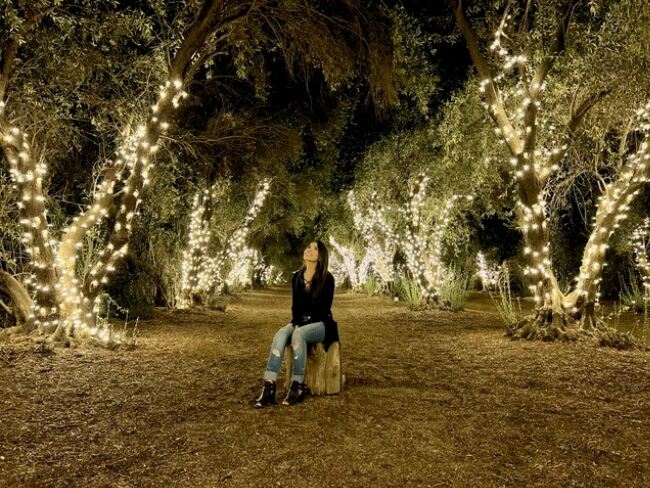
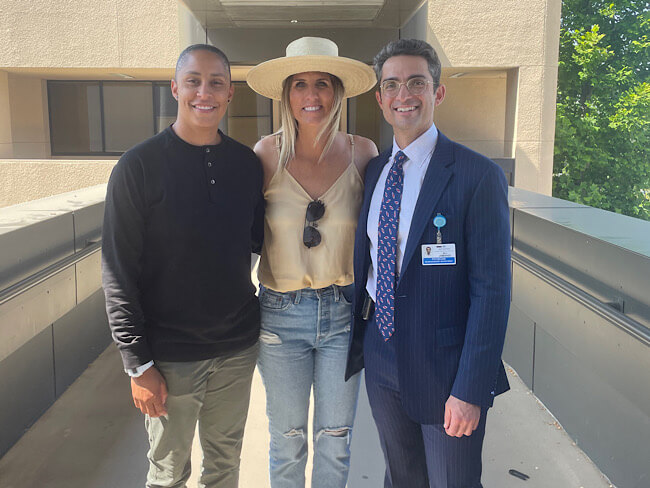
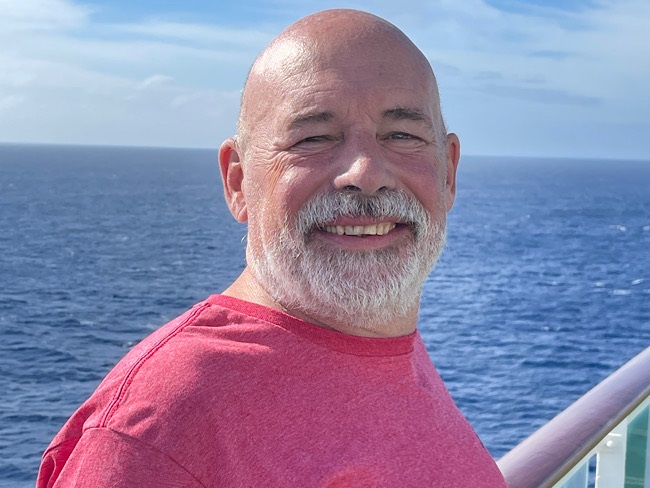
Adriana Sanchez-Ochoa is grateful she had the option of recovering at home after her bilateral mastectomy.
Adriana Sanchez-Ochoa learned she had breast cancer in both breasts. At first she wasn’t sure what to make of a suggestion from surgeon Brooke Vuong, MD. Dr. Vuong told her that she could have a double mastectomy and not spend a single night in the hospital. This was a surprise for the Northern California resident.
Her doctor and care team told her what to expect before, during, and after the surgery. They answered her questions and concerns until she was comfortable with the plan.
“My care team is amazing. The biggest factor with being ready to go home was how they prepared me,” said Sanchez-Ochoa.
A better experience after surgery
Many surgery patients prefer recovering at home. Avoiding a hospital stay can mean more comfort, preferred meals, and better sleep. For a long time it had been the norm for mastectomy patients to stay the night in the hospital, said Dr. Vuong.
“As surgeons, we would visit our patients the next morning, and they would usually be ready to go,” Dr. Vuong said. “We thought, what’s the added benefit of staying overnight?”
Kaiser Permanente began an initiative in 2017 to give patients the choice to recover at home without an overnight stay in the hospital.
I don’t remember feeling any pain. And there’s nothing like being at home. Adriana Sanchez-Ochoa, Kaiser Permanente member
The option builds on Kaiser Permanente’s Enhanced Recovery After Surgery program. Instead of the traditional fast before surgery, patients can have a carbohydrate drink. The program also reduces opioid use. Instead, patients receive local anesthetics and mild pain relievers, such as Tylenol. Patients are also encouraged to walk soon after surgery, if appropriate.
Care teams tell patients and caregivers what to expect at home, including how to manage surgical drains. The teams follow up with patients at home by phone, video, or secure messaging.
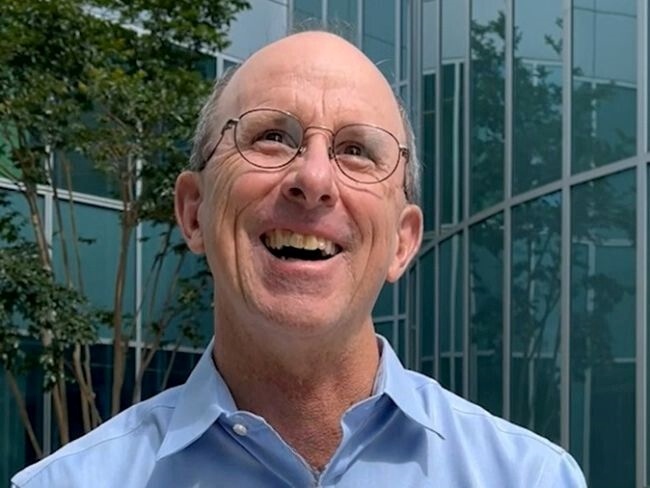
“We make sure patients have excellent pain management and know what to expect before and after surgery. And we want them to know how to get hold of their care team after hours, if necessary,” said breast surgeon Gillian Kuehner, MD.
A 2019 study looked at the program’s impact in the first 6 months. Home recovery rates for Northern California mastectomy patients grew from 23% to 61%. There were no significant changes in emergency department visits, reoperations, or readmissions. The program earned Kaiser Permanente the NCQA Innovation Award. The program received recognition for improving value and quality of care.
Growing interest during COVID-19
As of early 2024, 92% of our mastectomy patients in Northern California have used this option. It is also available to Kaiser Permanente patients in other areas. The COVID-19 pandemic highlighted new benefits of this approach. It helps open up beds for patients who need more immediate attention.
For Sanchez-Ochoa, going home after her mastectomy was “the best decision that I made.”
“I don’t remember feeling any pain,” she said. “And there’s nothing like being at home.”
Learn more about cancer care at Kaiser Permanente.
-
Social Share
- Share Recovering at Home After a Double Mastectomy on Pinterest
- Share Recovering at Home After a Double Mastectomy on LinkedIn
- Share Recovering at Home After a Double Mastectomy on Twitter
- Share Recovering at Home After a Double Mastectomy on Facebook
- Print Recovering at Home After a Double Mastectomy
- Email Recovering at Home After a Double Mastectomy

May 19, 2025
Member praises 50 years of collaboration with care teams
Karen Hansen’s doctors and clinicians have partnered with her to customize …

May 7, 2025
How to cope with anxiety after childbirth
As a new mother, Cherissa Ong was overwhelmed by stress. A mental health …

April 30, 2025
From fighter to father: How addiction care changed his life
Travis Taylor has substance use disorder and mental health conditions. …

April 25, 2025
Treating the heart and lungs together for a rare disease
With her medical teams working together, Sirina Hazeem is getting her life …

March 27, 2025
Living proof: Colon cancer highly treatable if caught early
There is an alarming rise in colon cancer rates among younger adults. Cynthia …

March 7, 2025
High blood pressure during pregnancy is on the rise
The keys to preventing cardiovascular conditions during pregnancy are knowing …

March 7, 2025
Kaiser Permanente in Hawaii cures 1,000th patient with hepatitis C
The milestone highlights its Viral Hepatitis Clinic's crucial role in addressing …

February 27, 2025
‘The heart attack that saved my life’
A sudden heart attack led Mark Twichel to seek care at Kaiser Permanente …

February 26, 2025
Colon cancer: Do you need to be screened?
If you’re age 45 or older, getting checked regularly for colorectal cancer …

February 18, 2025
I just need a chance
Billy Cardosi spent his life putting his family and job first. Then a heart-rela …

February 14, 2025
A fulfilling life on the other side of ovarian cancer
As a wife and a mother, Autumn Gray was determined to beat cancer to be …

February 12, 2025
Back on track after a rare cancer diagnosis
After facing sarcoma at age 18, drag-racing champion Cooper Chun needed …

February 4, 2025
What is therapy, anyway?
At Kaiser Permanente, our care is personalized for each patient's mental …

January 24, 2025
Is one drink a day OK? Here’s what to consider
NPR

January 15, 2025
After surgery, home was where his heart was
Virtual cardiac rehabilitation offers Mike Erskine a convenient, safe way …

January 13, 2025
How to prevent cervical cancer
Cervical cancer is highly preventable. HPV vaccination and regular screenings …

December 26, 2024
How telehealth can make life easier for people with cancer
Virtual care connects cancer patients like Rob Tufel to a wide range of …

November 26, 2024
How to reduce your risk of stroke
A Kaiser Permanente doctor and researcher shares the simple changes you …

November 22, 2024
Breast cancer survivor encourages early testing
Tasha Champion shares how early testing by her oncologist at Kaiser Permanente …
November 18, 2024
The power of early detection and proactive men’s health
A father's determination to stay healthy for his 3 children led him to …

November 13, 2024
Self-care for caregivers matters: Here’s why
A sharp increase in rates of adult caregiving is taking a mental and physical …

November 12, 2024
Surviving lung cancer as a nonsmoker
As a lifelong nonsmoker, Mariann Stephens was shocked to learn she had …
October 29, 2024
That’s not tennis elbow
A Kaiser Permanente physician thought he pinched a nerve during a tennis …

October 15, 2024
107-year-old member credits Kaiser Permanente for longevity
Bettye Garrett’s personal doctor says her healthy perspective on life’s …

October 8, 2024
It started with a bad feeling
In August 2023, John Lynn collapsed at work. For the next year, he fought …

October 4, 2024
Teacher learns about herself and how to live with anxiety
A lifelong educator seeks behavioral health care to manage repetitive worries, …

October 1, 2024
Screening for breast cancer: Mammogram guidelines
A Kaiser Permanente radiologist answers commonly asked questions.
October 1, 2024
From depression to connection: Older adult finds her way
After a long period of loneliness and isolation, Roberta Maguire gets the …
September 20, 2024
Ovarian cancer journey confirmed nursing student's calling
Miriam Gutierrez was diagnosed with late-stage ovarian cancer at age 31. …

September 19, 2024
First look at new Lakewood facilities
New medical offices will enhance the health care experience for members …

September 18, 2024
More than 100 ‘Top Docs’ recognized in Washington state
Kaiser Permanente celebrates doctors and nurse practitioners recognized …

September 18, 2024
Cancer rates are rising in younger age groups
‘Connect’ with research to help understand more about the increase of certain …

September 17, 2024
A Latina’s voice in mental health is impactful with her clients
Connecting through a shared heritage gives one therapist a unique perspective …

September 17, 2024
Playing on after 2 decades of cancer care
With the support of his health care team and nurse navigator, musician …

September 17, 2024
Groundbreaking at new medical offices in Pueblo
The new Pueblo North Medical Offices will replace the existing facility …

September 6, 2024
Navigating a world turned upside down after heart failure
After a life-threatening series of heart attacks at age 57, Bunnell Fockler …

August 29, 2024
After Stage 4 ovarian cancer, she’s still going strong
Donna Budway received prompt surgery followed by chemotherapy. She credits …
August 29, 2024
Neurosurgery and a deep, enduring doctor-patient relationship
A basketball coach’s remarkable story of undergoing brain tumor surgery …

August 28, 2024
Making breastfeeding work: A second-time mom’s journey
Support from a dedicated care team helps Tiffany Anonye breastfeed her …

August 28, 2024
Final beams placed at Parker Medical Offices
The final steel beams for the new Kaiser Permanente Parker Medical Offices …

August 27, 2024
From sore throats to ice cream floats
A mother and daughter share a special bond after undergoing tonsillectomies …

August 26, 2024
Katie's ride: Motorcycle rally a surprise for patient
Kaiser Permanente in San Diego helped plan a special send-off for Katie …

August 15, 2024
Back home one day after heart surgery
Ed Dalmasso needed an aortic valve replacement. His care team provided …

August 6, 2024
For a father with prostate cancer, knowledge is power
Harold Newman had advanced prostate cancer. Genetic testing helped expand …

August 1, 2024
Kaiser Permanente tops Colorado ‘Top Doctors’ list
5280 Magazine named 332 Kaiser Permanente physicians to its annual Top …

July 10, 2024
We help members lower their risk of heart attacks and strokes
A Southern California program, powered by our connected care model, is …

June 25, 2024
Prompt postpartum care saves a baby’s life
When a newborn was diagnosed with meningitis, a life-threatening infection …

June 17, 2024
That’s a lot of babies!
Delivering multiple babies is difficult, but Kaiser Permanente care teams …

June 17, 2024
A culture of caring eases a cancer journey
Exceptional, personalized radiation oncology care helped Maura Craig treat …

June 13, 2024
Conquered 2 cancers while climbing mountains
Chris Hogan faced kidney cancer and prostate cancer at the same time. He …

June 3, 2024
A call to ‘Connect’ for cancer prevention research
Participate in a study to help uncover the causes of cancer and how to …

May 31, 2024
Stage 4 lung cancer: A story of hope
A young father is enjoying “bonus time” with his kids thanks to new targeted …

May 21, 2024
Surviving stage 4 lung cancer with immunotherapy treatment
Patients like Carol Pitman are living longer thanks to advances in lung …

May 10, 2024
Self-care is key for new parents
Feeling emotional or overwhelmed after a new baby’s arrival? You’re not …

May 7, 2024
Making cancer care more convenient in Southern California
Kaiser Permanente has opened a new Radiation Oncology Center at the Bellflower …
May 1, 2024
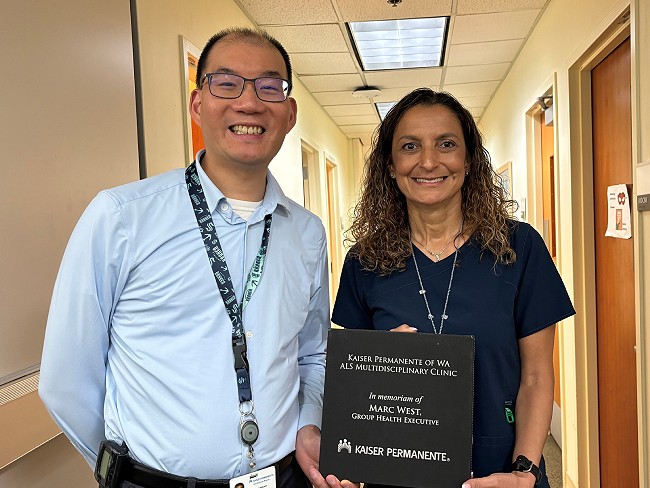
Tacoma ALS clinic recognized for high-quality care
Patients with amyotrophic lateral sclerosis, also called Lou Gehrig’s disease, …

April 17, 2024
5 common health conditions men don’t like to talk about
Some of the most common conditions affecting men carry a social stigma …

April 10, 2024
For a new mom, talking about her worries helped her heal
One in 5 people experience depression, anxiety, or other mental health …

April 9, 2024
Denver Fire Department annual blood work screenings triple
It’s easy to put off recommended health screenings, and sometimes even …

April 8, 2024
Reducing inequity with fruits and vegetables
Black Americans experience worse health outcomes compared to other populations. …

April 1, 2024
Lynch syndrome: Managing the risk of hereditary colon cancer
Lynch syndrome is a gene mutation that increases colon cancer risk. Learn …

March 29, 2024
Faster recovery: From cardiac scare to exploring Italy
Virtual cardiac rehab helped Mike Kelly heal at home after a life-threatening …
March 20, 2024
Life after cancer: Surviving and thriving
A healthy life after cancer is possible. Learn how Kaiser Permanente helps …

March 14, 2024
Healthy kidneys support overall good health
Kaiser Permanente excels in preventing, detecting, and treating kidney …

March 14, 2024
Midwife offers personal care for mom facing complications
For Sam Beeson, having a midwife at her side during her pregnancy helped …

March 12, 2024
In-home recovery restores harmony to life
Colorado musician back with the band thanks to new virtual cardiac rehab …

March 6, 2024
Joining a national effort to test new ways to find cancer
As part of the Cancer Screening Research Network, our researchers will …

March 6, 2024
Are you dreading the spring season?
A new Kaiser Permanente facility in Bellflower, California, makes customized …

March 6, 2024
Colon cancer screening: She’s glad she didn’t wait
A timely preventive test reveals Rebecca Kucera has cancer. Swift treatment …
March 5, 2024
Researchers look for ways to find pancreatic cancer early
Early detection of the disease, before it becomes advanced, will increase …
February 22, 2024
The journey of a lifetime
Care teams at Kaiser Permanente Fontana Medical Center helped Phillip Crawford …

February 21, 2024
From planning his funeral to celebrating his wedding
Gabriel Abarca had no hope for his future. Then the team at Kaiser Permanente …

February 1, 2024
Take a break from cannabis while expecting, study suggests
Research shows that marijuana use during pregnancy increases health risks …

January 26, 2024
Retiree back in the swing of things after heart procedure
Tookie Gentilcore returns to enjoying life thanks to a quick, safe method …

January 24, 2024
A full-circle journey for one cancer survivor
Grateful for compassionate and successful Hodgkin lymphoma treatment at …

January 17, 2024
How diabetes can affect your heart
People with diabetes are more likely to have heart disease.

January 10, 2024
‘You don’t know unless you ask them’
Kaiser Permanente’s Patient Advisory Councils help us create exceptional …

December 19, 2023
Determined to drop the weight and stop the cycle of diabetes
Following a COVID-19-related hospital stay, Robert DeLeon took charge of …

December 15, 2023
Family-centered care, through pregnancy and beyond
Members experiencing a low risk pregnancy have the option of having their …

December 13, 2023
Nurse navigators guide patients from diagnosis to treatment
An unexpected cancer diagnosis left Jennifer Martin unsure of the next …

December 6, 2023
Leading research with gratitude
Learn how you can participate in a study to uncover what causes cancer …

December 6, 2023
Video prenatal visits are a boon for a busy working mom
A new care option offers a mix of in-person and virtual visits, supported …

December 1, 2023
Surviving — and thriving — after cancer
From diagnosis to recovery, David Parsons, MD, shares how screening, treatment, …

November 15, 2023
Care at home: Giving patients what they want
Our Advanced Care at Home program provides high-quality, safe care in familiar, …

October 25, 2023
Breast cancer during pregnancy: Caring for mom and baby
A team of specialists treats an expecting mother’s cancer while keeping …

October 24, 2023
Childhood anxiety: What parents need to know
A child and adolescent psychiatrist shares tips on supporting your child …

October 23, 2023
A renewed sense of purpose after surviving breast cancer
Joy Short, a Kaiser Permanente member and employee, turned her breast cancer …

October 11, 2023
Early breast cancer detection improves quality of life
For 75-year-old Peggy Dickston, a surprise diagnosis was caught early thanks …

October 3, 2023
Nursing excellence recognized at Fontana Medical Center
The prestigious Magnet® designation affirms the compassion, dedication, …

September 20, 2023
Healing after a heart attack
For years, serious heart attacks meant hours of weekly appointments. Now, …

September 19, 2023
Is telehealth right for you?
Members give video visits high marks — and with a few simple tips, you …

September 6, 2023
Recovery from addiction is possible
Our clinicians help patients get the care they need to move forward with …

August 29, 2023
Preventing overdoses starts with education
Risk factors are not always associated with addiction or substance abuse. …

August 17, 2023
Beyond clinic walls: Research supporting healthy communities
Stories in the Department of Research & Evaluation 2022 Annual Report demonstrat …

August 17, 2023
Cancer research: The role of immunotherapy
Research and clinical trials play a vital role in advancing cancer treatment …

August 16, 2023
Cervical cancer screening: Exploring the at-home HPV test
Kaiser Permanente is at the forefront of cervical cancer research. Find …
August 14, 2023
Tips for ensuring a safe and healthy college experience
Students should study up on their care options to ace their school experience. …

August 14, 2023
Marla’s story: Surviving acute promyelocytic leukemia
After a diagnosis for a rare type of blood cancer, Marla Marriott got high-quali …

August 10, 2023
Highlighting our community health work in Southern California
The Kaiser Permanente Southern California 2022 Community Health Snapshot …
August 4, 2023
Eating well and adopting healthy habits helps prevent cancer
Learn how lifestyle medicine is part of cancer care at Kaiser Permanente.