Having her ‘rainbow baby’ after a high-risk pregnancy
Remote perinatal monitoring and frequent in-person appointments helped Alicia Saunders deliver a healthy baby boy.
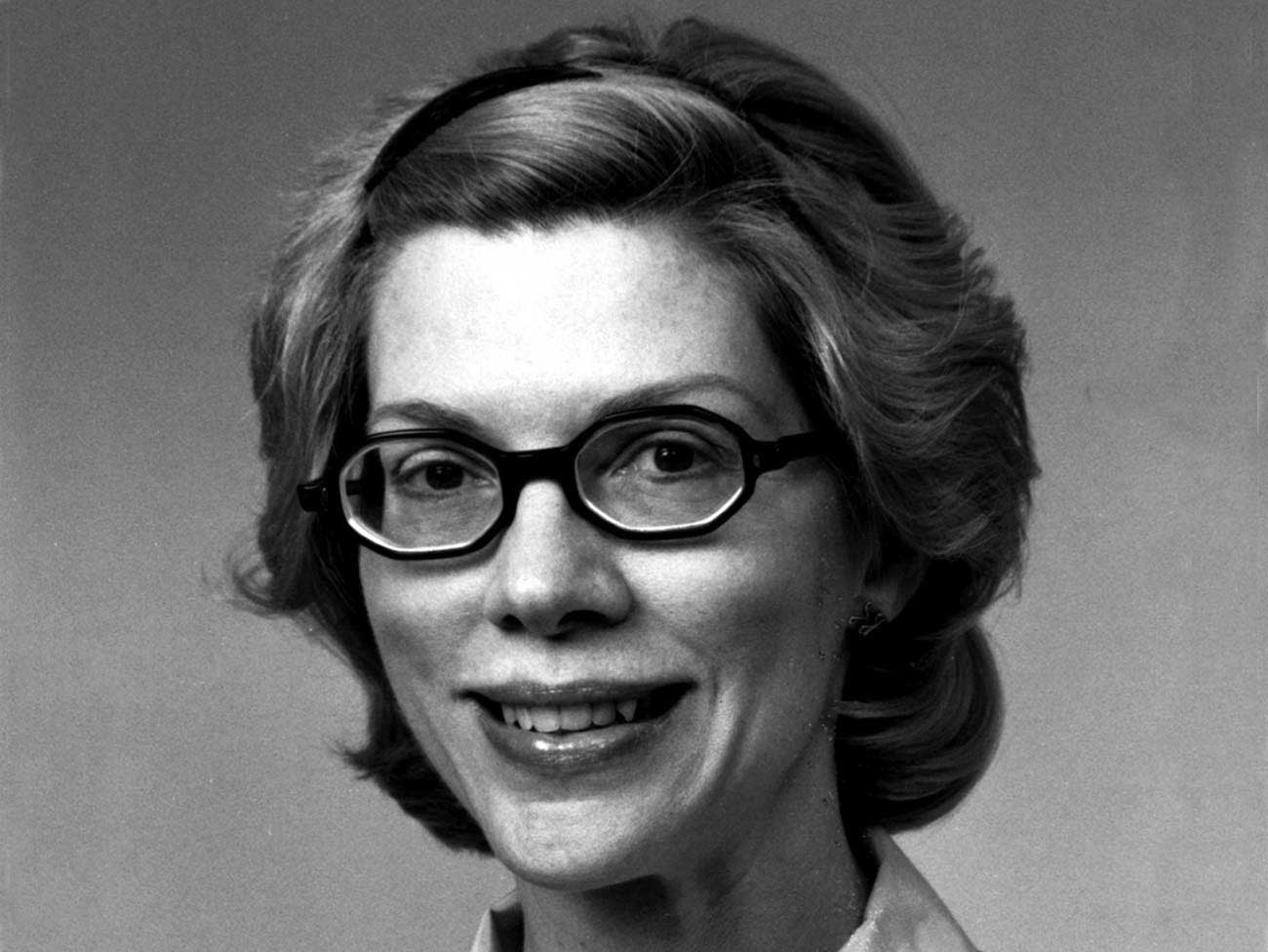
Alicia Saunders and her husband, David, and daughter Zoe welcomed Kody in 2021.
Alicia Saunders felt a mix of emotions when she learned she was pregnant with her third child.
Less than a year earlier, her second child, Olivia, had been stillborn because of an umbilical cord abnormality, and the pain of that loss was fresh for Saunders. Adding to her worry was the knowledge that her third pregnancy was high risk because of her age (36), a diagnosis of gestational diabetes, and her history of preeclampsia (a pregnancy complication characterized by high blood pressure).
Remote monitoring of high blood pressure and diabetes
An innovative remote perinatal monitoring program helped ease her worries. Saunders was given Bluetooth-enabled blood pressure and blood sugar monitors to use at home. The devices transmitted readings to her electronic health record through an app on her smartphone, allowing her care team to monitor the health of her pregnancy between office visits.
“Being pregnant after a loss is a lot, both physically and emotionally,” said Saunders. “I definitely appreciated having more frequent contact with my care team.”
Saunders began each day by checking her blood pressure and blood sugar. She repeated that process after meals and before she went to sleep.
“If any of my numbers was high or low, I would get a phone call,” she said. “And if the nurses were still concerned after asking me some questions, they would tell me to come in.”
Black women face increased risk
High blood pressure and diabetes during pregnancy create risk for both mother and baby. The prevalence of these conditions is one of many factors that contributes to the United States’ high rate of maternal mortality. Black women have higher rates of hypertension and diabetes than white women and are also 3 times more likely to die from pregnancy-related causes.
“Remote monitoring has been transformative in how we’re able to manage high-risk patients like Alicia,” said Bindu Bareddy, MD, Saunders’ ob-gyn at Kaiser Permanente in Georgia.
“Going to a doctor’s appointment can take half a day,” she added. “That’s difficult for patients who work or have children when all that may be needed is to check their blood pressure or blood sugar level. This program improves convenience for our patients and lets us be present in their care even outside of scheduled appointments.”
Frequent in-person appointments for high-risk moms
While remote monitoring provides important virtual touchpoints, it doesn’t take the place of in-person visits.
“We start out seeing our high-risk moms every 4 weeks. That accelerates to every 2 weeks, then weekly, and by 32 weeks, we’re seeing them twice a week,” said Dr. Bareddy. “We check the baby’s heartbeat, look at the amniotic fluid, and if we see anything concerning we send the mom on to a high-risk specialist.”
Saunders appreciated the reassurance these appointments provided. “A couple of times, if the baby wasn’t moving as much, my husband and I would get scared, and we’d go in. The care team never made me feel like I was overreacting. They told me, ‘You can come in as often as you want or need.’”
A healthy baby boy
Saunders’ anxiety grew as her pregnancy approached 36 weeks, when Olivia’s stillbirth had occurred. At 35 weeks, Saunders gave birth to Kody, a healthy baby boy.
“A rainbow baby is a baby born after a loss,” she explained. “Kody is our rainbow baby, and I think he knew how much we needed him to get here.”
Now the mom of a busy toddler (along with firstborn Zoe and Nyanna, who joined the family through adoption), Saunders serves on 2 patient advisory councils at Kaiser Permanente. The councils are focused on enhancing perinatal safety and improving the maternity experience for people of color.
“I personally experienced a high-risk pregnancy, and I benefited from remote monitoring,” she said. “It makes me jump for joy to know that other moms will have that peace of mind.”