Critical care and support for our youngest patients
In Oregon, specialists and parents come together to design a specialized care plan for babies in the neonatal intensive care unit.
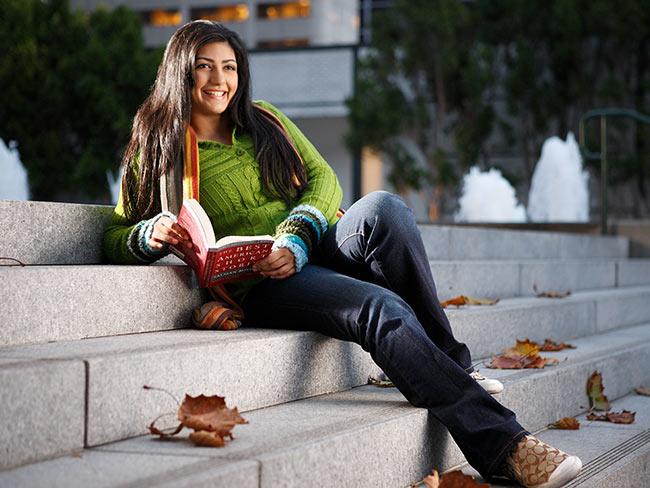
Kim Anderson and her son, Hakan, who was born premature but quickly grew stronger with 24-hour care. Anderson now helps new parents navigate the NICU.
When Kim Anderson’s son, Hakan, was born premature in 2018, he weighed just 4.6 pounds and struggled to eat. “He would fatigue very quickly when he would nurse, so they tube- and bottle-fed him so he could grow,” said Anderson.
Anderson and her husband talked with the medical team and they determined that Hakan needed to be admitted to the neonatal intensive care unit, or NICU, at the Kaiser Permanente Sunnyside Medical Center.
Having a child in the NICU can be stressful for new parents. It’s not the quiet, warm nursery many parents plan for their newborn. It’s a high-tech facility, filled with strange equipment, lights, monitors, noises, and more.
It’s also filled with teams of neonatal specialists working around the clock to provide the best care possible for the babies in their unit.
“I would get up and get there by 8 a.m. and then leave at 8 p.m.,” said Anderson. But she felt confident in the nurses caring for Hakan when she wasn’t there and developed a strong rapport with them when she was.
I got to be part of every decision, and I felt very included in Hakan’s care. The nurse let me give him his first bath, and I asked them to teach me how to use the feeding tube so I could help. Kim Anderson, Portland, Oregon
A lifeline for parents and babies
“Parents are an important part of the NICU team,” said Jennifer Marsh, RN, NICU charge nurse at Sunnyside Medical Center. “We help them to be with their baby, to bond, as much as possible, while making sure their little one gets the specialized care needed to get well.”
“I got to be part of every decision, and I felt very included in Hakan’s care,” Anderson said. “The nurse let me give him his first bath, and I asked them to teach me how to use the feeding tube so I could help.”
After 2 weeks, Hakan had grown and was eating well enough to go home. Today, he’s “adorable, fun, silly, and kind.” And while he just celebrated his fifth birthday, the NICU is still close to Anderson’s heart.
Giving back to care for others
So, when a parent partner program began 2 years ago to improve NICU care based on feedback from families who’d been there, Anderson signed up.
The program connects people like Anderson with Kaiser Permanente caregivers, social workers, and managers so they can share ideas about how to improve the patient experience in the NICU.
“I had wonderful care in the NICU, and I felt this was a way to give back,” said Anderson, who says the program creates an avenue for parents to share their unique experiences.
“Our experience is so profoundly different from the parents’ experience,” said Marsh, who helps lead the patient partner program. “Hearing from them is very enlightening, and it makes us want to do better and come up with organic solutions for them.”
A profound impact
Conversations have led to changes that are already improving the parent experience.
Participants in the program established a mentor program that matches families who currently have a child in the NICU with people who’ve been through it.
Other projects are more festive, such as the revival of reunions for staff and the families of NICU graduates.
“As a caregiver, I can have a profound impact on a family’s experience as they live through a stressful period with their newborn in the NICU,” said Marsh. Through this program, NICU families will help lead the way.
Learn more about the Neonatal Intensive Care Unit (NICU) at Kaiser Permanente