Pharmaceutical marketing hurts patient care
At Kaiser Permanente, our doctors and pharmacists work together to ensure the drugs we prescribe are based on the evidence, not ads.
Prescription drugs are unaffordable for too many patients.
Prescription drug manufacturers spend an inordinate amount of money marketing their products to doctors and patients alike. The tactics are intended to influence patients toward expensive drugs — even when equally effective, lower-priced products are available.
In 2024, the United States spent over $800 billion on prescription drugs. At the same time, 1 in 4 patients reported having trouble affording their medications.
Pharmaceutical marketing drives up the cost of prescription drugs. And patients with health insurance often don’t see the full cost. They may just pay a fraction, while insurance covers the rest. Even doctors might not realize the expensive price of these drugs.
The result? Drug costs are draining patient, government, and health system resources.
Direct-to-consumer advertising
Pharmaceutical ads are, in many ways, unusual and unique.
All ads entice you to buy a product. But when you see a prescription drug ad, you can’t just go out and buy the product. You first need an appropriate assessment of your health and condition. And you need to work with a doctor to determine if that drug is right for you, or if other options may be better for care.
Your doctor uses medical expertise and considers your symptoms and health history to help make the decision. Even so, pharmaceutical companies spent nearly $14 billion on direct-to-consumer advertising in 2023.
TV and social media are flooded with drugs ads. Patients see these ads and may pressure their doctor to prescribe a drug — regardless of effectiveness, safety, or price.
Drug companies know this strategy works. One survey found that 1 in 8 adults was prescribed a specific drug after seeing it in an ad and asking their doctor about it.
But purchasing a drug does not necessarily translate into value. The drug might be less effective, less safe, and more expensive than other options.
A study in JAMA Network found that less than a third of drug ads focus on high-value drugs, which are drugs that are proven to work at a reasonable price. In other words, most ad dollars go toward promoting drugs that aren’t necessarily the most effective, safe, or affordable.
The rise of telehealth prescribing
Recently, direct-to-consumer telehealth companies have risen in popularity. Many of these companies specialize in prescribing medications that treat specific conditions, such as obesity, hair loss, acne, and anxiety.
This kind of telehealth prescribing coupled with advertising has opened new avenues to reach even more consumers.
Consider the dramatic rise in demand for anti-obesity medications.
- Direct-to-consumer telehealth companies advertise the drugs.
- These companies use a third-party telehealth platform to allow patients to meet with a doctor who will prescribe the medication. In some cases, the medications may be prescribed for patients when they’re not medically appropriate, rather than for patients who have a high body mass index or other weight-associated health condition, such as diabetes.
- The result has been a dramatic increase in sales for these drugs.
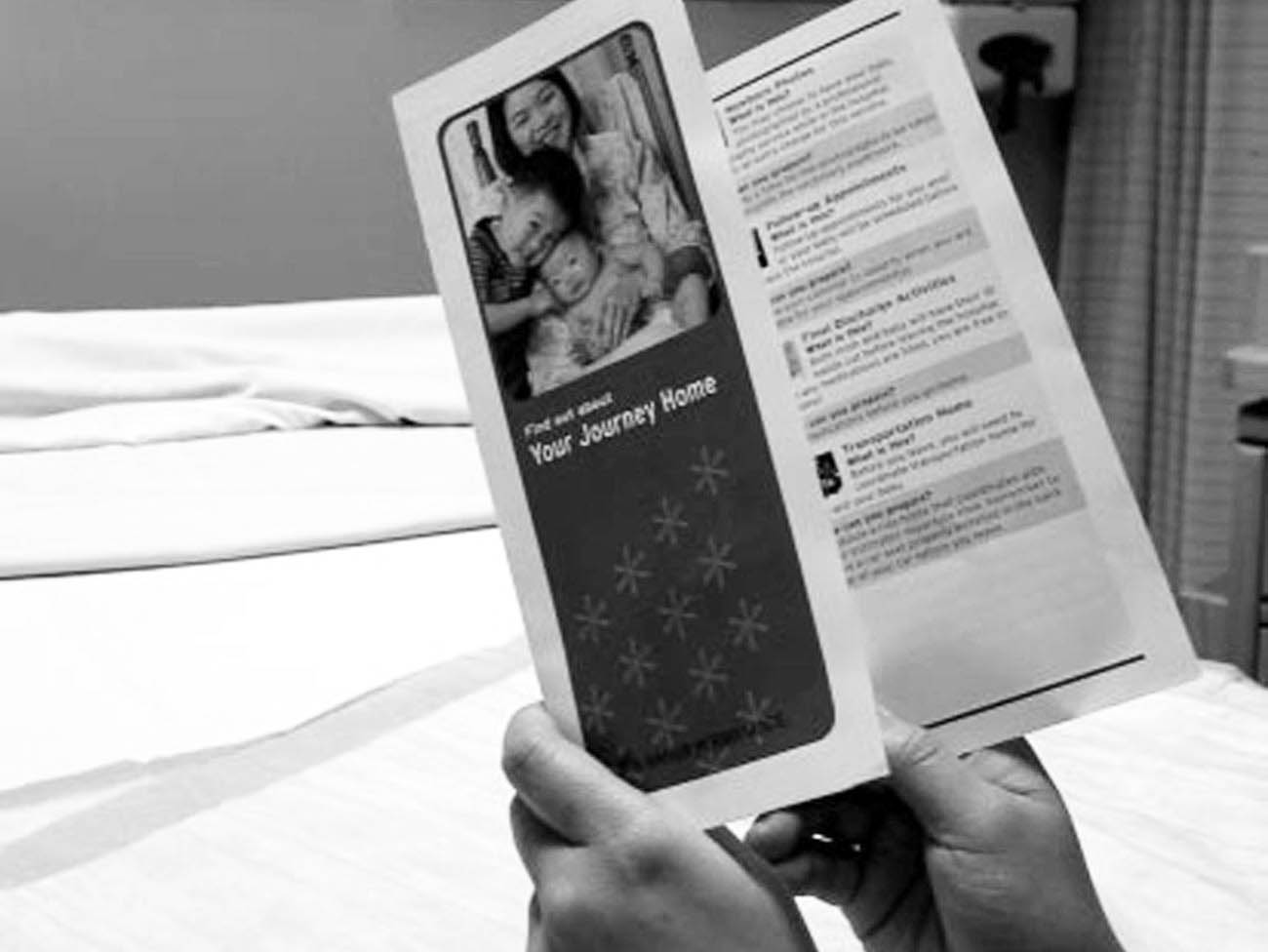
The use of direct-to-consumer telehealth providers can present other challenges.
- Patients may see clinicians who don’t know them or their health history the way their usual primary care doctor does.
- Important details about the visit and any medications prescribed don’t go into their electronic health record.
- Gaps in care and potential safety concerns can result.
Recently, some drug companies even launched their own direct-to-consumer telehealth platforms. They allow a patient to consult with a doctor who is not their usual doctor and get a prescription for the company’s weight-loss drug. A third-party pharmacy then fills the prescription.
The drug company runs the platform and shapes the whole experience. But it begs the question whether the best medical care can be provided in such a setting.
A better approach
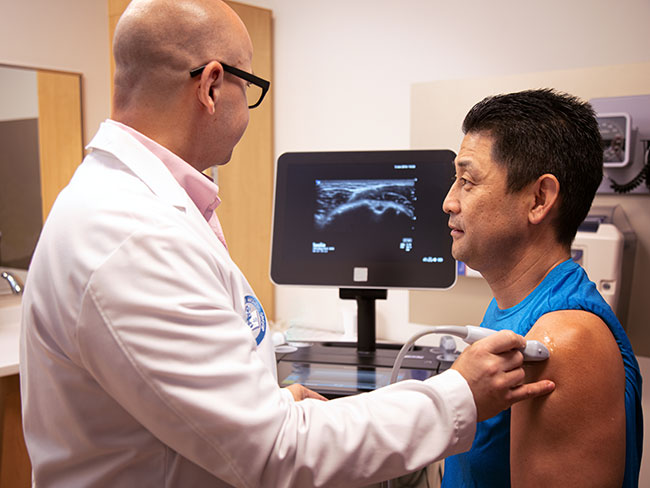
At Kaiser Permanente, we use evidence-based guidelines and processes to educate our doctors and other prescribers on the safety and efficacy of drugs.
We have a team of clinical pharmacist experts that independently review all available materials, data, and evidence on a drug. We also review our own internal data to assess how drugs perform over time.
Instead of allowing pharmaceutical sales representatives to enter our hospitals and medical offices, we rely on our own pharmacy education staff to help doctors stay current on the most-effective drugs. They may use peer-to-peer education, direct in-person and virtual visits with doctors, and presentations to specialist groups.
Our evidence-based approach to prescribing ensures patients receive high-quality, high-value treatment.
Curbing pharmaceutical marketing
Policymakers must act to combat the negative effects of pharmaceutical marketing. They should:
- Restrict TV and online drug ads
- End tax breaks used by drug companies for their drug ads
- Require drug sales reps to get certified by the state before they’re allowed to promote medications to doctors
- Require robust, long-term evidence for safety and efficacy to secure FDA approval for drugs
Meanwhile, independent, research-based organizations like PharmedOut play an important role in educating the public on the many ways pharmaceutical companies advertise and influence prescribers and patients.
Patients deserve to have medications prescribed based on evidence, not splashy commercials.