Buprenorphine saves lives. Why can’t more patients get it?
Policy changes are crucial for better opioid addiction treatment.
Expanding access to buprenorphine will strengthen both lives and the country.
As an addiction medicine physician, I am honored every time my patients trust me enough to share their life stories — to let down their guard and know that I hear them and will do everything I can to help them overcome addiction.
This trust is the core of what makes addiction care possible. It also comes with a responsibility to provide patients with the best care and treatments available.
The recent, meaningful reduction in overdose deaths over the last few years offers hope, but the crisis continues. Across America, doctors face big challenges in meeting this responsibility.
Effective treatments are often out of reach due to barriers like stigma or outdated rules. These challenges are compounded by the ongoing illicit fentanyl epidemic and a rise in unregulated substances like Kratom, which are easier to find.
Opioid-use-disorder treatments are a prime example of this challenge. The prescription medication buprenorphine offers one of the greatest opportunities in addiction care but is often out of reach.
Buprenorphine’s role in opioid treatment
Buprenorphine is an opioid approved by the U.S. Food and Drug Administration to treat pain and opioid-use disorder.
Its special properties make it both effective and safe for treating addiction by:
- Reducing cravings and withdrawal symptoms by partially activating brain receptors
- Lowering the risk of overdose from drugs like fentanyl by blocking brain receptors
- Blocking other opioids, stopping them from causing a high
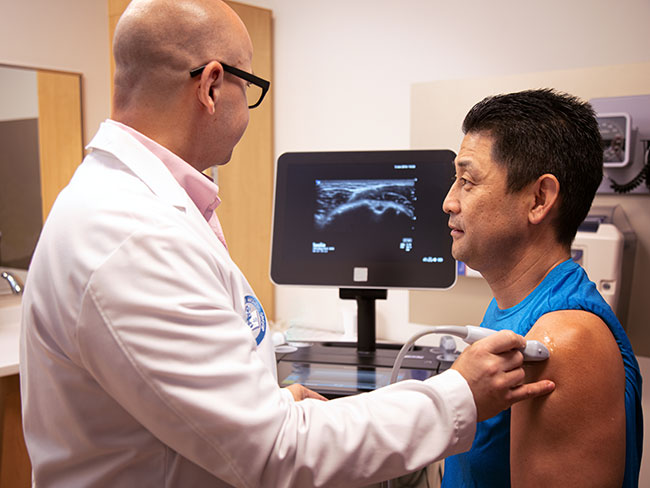
These traits make buprenorphine an important treatment option. At Kaiser Permanente, our comprehensive treatment plans often include medication like buprenorphine, therapy, and peer support. This approach ensures patients get the care they need for effective recovery.
Barriers to buprenorphine treatment
Although buprenorphine is safe and effective, many doctors still don’t prescribe it. Before 2023, this was largely due to a federal rule, known as the “X-waiver,” that required extra training and certification — requirements not needed for similar medications.
Removing the requirement was key. But more action is needed to increase access to buprenorphine for people addicted to opioids.
Remaining barriers to buprenorphine treatment include:
- Geographic disparities: Many areas, especially rural communities, lack buprenorphine prescribers. Often this is due to a shortage of professionals and professional hesitancy to prescribe. This leaves 3 in 10 Americans who live in rural areas without access to the essential treatment.
- Racial disparities: Opioid overdose deaths among Black people have surged, especially among Black males. From 2010 to 2020, these deaths increased eightfold. Opioid death rates are now higher among Black people than white people. Despite this, Black patients are less likely to receive buprenorphine than white patients.
- Provider hesitancy and stigma: Many doctors and other health care professionals feel unprepared to prescribe buprenorphine, partly due to insufficient training. Stigma surrounding addiction treatment also plays a role. Additionally, a lack of basic information about buprenorphine means many health care professionals are unaware they can prescribe this essential treatment.
- Reporting requirements: Buprenorphine, a Schedule III drug, may be treated similar to Schedule II opioids by distributors, including the requirement for increased reporting. Reporting requirements can add complexity to the dispensing process. Requirements may also lead some pharmacies to avoid offering the treatment, fearing that their dispensing patterns may be viewed negatively.
- Cost barriers to long-acting injectable buprenorphine: Long-acting injectable options can be highly effective and support sustained recovery. Yet, for many patients their cost is too much. Sustainable pricing for these products is necessary to significantly expand access.
Removing these barriers is essential. Doing this will strengthen health care in our country by:
- Improving patient care: People who take buprenorphine are at lower risk for fatal overdoses. The treatment also helps people recover from opioid addiction.
- Reducing U.S. health care spending: The treatment makes patients less likely to need costly emergency care and long-term residential care.
- Boosting the health of our communities: When people with opioid use disorder get the right treatment, drug use falls, crime rates drop, and families and communities flourish.
Policy changes to increase access
Policymakers can help more people benefit from buprenorphine. They can peruse policy changes that:
- Make prescription of buprenorphine through telemedicine permanent: Preserve the use of audio and video visits and the option to provide an initial supply before an in-person visit. This will help ensure patients can begin care the day they ask for help.
- Expand prescriber eligibility: Broaden the role of clinical pharmacists to provide evidence-based treatment options for opioid-use disorder, including by allowing them to prescribe buprenorphine.
- Increase facility access: Buprenorphine should be more widely available in correctional and residential facilities. Public policies can ensure that people at high risk of overdose get treatment.
- Bolster existing trainings: Drug Enforcement Agency training programs for health care professionals should include specific information about buprenorphine. This addition will help reduce stigma, increase awareness, and encourage more health care professionals to offer the treatment confidently and compassionately.
- Distinguish between buprenorphine and other opioids: Policymakers should enhance messaging that buprenorphine is a Schedule III medication and should be treated differently from other opioids, which are Schedule II medications. This distinction should be made when safeguards are established and implemented as part of manufacturer-controlled safety procedures, algorithms used for opioid distribution to pharmacies, and pharmacies’ automated checks.
Implementing these policy changes is crucial. By making buprenorphine more available, we can save lives and strengthen communities.
It’s time to ensure everyone can get the help they need to overcome addiction.