Solutions for strengthening the mental health care workforce
Better public policies can help address the challenges. We encourage policymakers to focus on 4 key areas.
Through investments and collaboration, health care stakeholders and policymakers can improve access to care.
Demand for mental health care services is high and rising.
More than 1 in 3 people live in an area with a shortage of mental health professionals. Communities of color and people in lower-income areas are most affected. People who live in economically stressed cities and rural areas face the greatest challenges accessing care.
Addressing this crisis requires growing our mental health workforce. To do that, health care stakeholders and policymakers must come together to improve how our country recruits, trains, licenses, and places mental health professionals.
Growing the workforce is crucial
Federal and state governments should engage health care organizations, academic institutions, and community leaders to develop and expand the mental health workforce. Working together, we can find solutions that equitably serve all communities.
At Kaiser Permanente, we recommend 4 key focus areas for policymakers:
- Career path promotion: Introducing mental health career paths in high schools will inspire the next generation of mental health care professionals.
- Professional licensing: Streamlining licensure requirements will expedite the entry of qualified professionals without compromising care quality. One change we recommend is facilitating licensure for individuals licensed and in good standing in other states, such as through interstate licensure compacts for mental health professionals.
- Financial incentives: Government programs should offer scholarships, loan forgiveness, and stipends that would lower financial barriers and attract a wider pool of candidates to the mental health field. A specific area of attention should be to increase and restructure graduate medical education funding with a focus on psychiatry, child psychiatry, and addiction medicine residency positions and fellowships.
- Workforce diversity: Recruiting and training diverse and multilingual clinicians should be a national priority.
Aligning the workforce with demand
As the mental health care workforce grows, it’s vital that health care organizations and advocates ensure equitable access to care. This can’t be achieved if too many clinicians pursue private practice with an intent to serve primarily people who can afford to pay out of pocket.
To promote equitable access, policymakers must enable and support organizations serving diverse populations, such as Medicare, Medicaid, and commercially insured patients, in hiring and retaining therapists.
We also must reduce the unnecessary challenges many new graduates face on the path to licensure. Many find it difficult to complete their supervised hours.
For example, in several states, aspiring mental health professionals need over 4,000 hours of supervised work experience after graduating to receive their license to practice. That amounts to 2 years of full-time work. Graduates also often aren’t paid well for these hours — some even have to pay for their supervision. And, that’s if they can find supervision opportunities, which are not widely available. This barrier keeps many people from entering the profession or pursuing their license, especially those with lower incomes and fewer resources.
A promising approach adopted by some states involves granting provisional licenses to new graduates after they pass their exams. These licenses enable new clinicians to start providing care under the supervision of experienced licensed professionals.
We endorse this approach. It supports new professionals and ensures patients receive high-quality health care. We recommend more states consider this approach to quickly expand the mental health workforce.
Improving access through telehealth
In addition to growing the workforce, we need to ensure services are widely accessible. The COVID-19 pandemic demonstrated the power of telehealth to provide effective access to all kinds of health services, but particularly mental health services. More can be done to promote it.
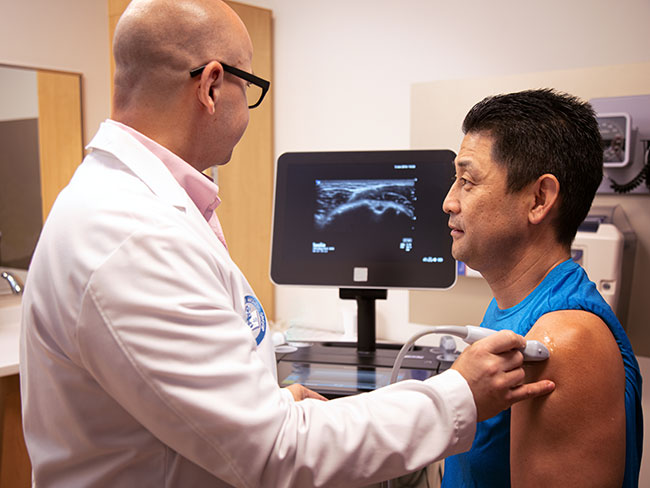
At Kaiser Permanente, both patients and clinicians tell us they often find telehealth sessions more convenient and comfortable. We see this in our data: Few patients cancel or miss their phone and video appointments.
Recent studies, including one from the Substance Abuse and Mental Health Services Administration, show the effectiveness of telehealth for treating people who have substance use and mental health disorders.
It’s essential to keep improving and expanding telehealth, especially for people who could benefit most from it. A key role for policymakers is ensuring everyone has internet access, especially in areas with a shortage of mental health workers.
Policymakers should also change rules, like requiring in-person visits, that unnecessarily limit the use of telehealth. Supporting the use of telehealth across state lines to expand coverage will also help bring care to people in rural and underserved areas.
Investing in future therapists
Kaiser Permanente is investing in workforce development to serve our members and communities. Here are a few ways:
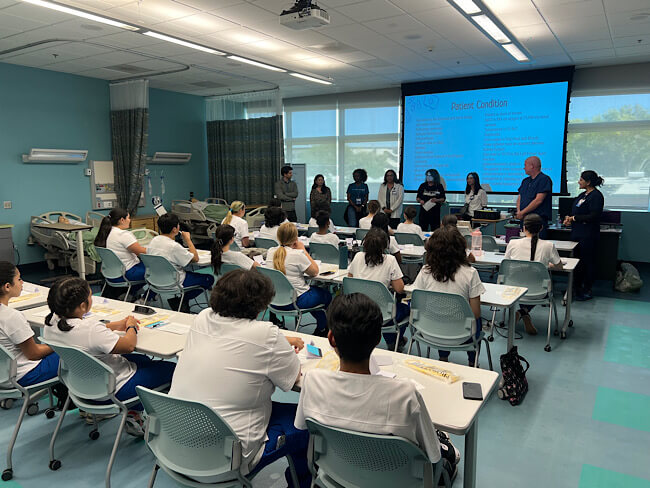
- Mental Health Scholars Academy: Backed by a $30 million investment, this program supports our employees in obtaining advanced degrees in mental health fields. By offering scholarships, mentoring, and access to clinical hours, we are nurturing a new generation of professionals. Reflecting our focus on promoting diversity in the professions, over 77% of participants are people of color, and nearly 40% are bilingual.
- Kaiser Permanente Mental Health Training Program: With more than 300 trainees annually, this is the largest nongovernmental program of its kind in the U.S. The breadth of our program allows trainees to obtain training at any level, from pre-degree to post degree, or to complete all components of their training with us from practicum to licensure. It shapes future mental health professionals through diverse and rigorous training experiences, ensuring comprehensive and culturally sensitive care.
- Post-master’s degree associate programs: These programs offer mental health graduates in Oregon and Washington a way to complete their supervised clinical hours, including some that provide wages and benefits. The programs also focus on following evidence-based practices and promoting equity and diversity. By the end of 2024, we plan to have similar associate programs in every state where we provide care.
- Kaiser Permanente Mental Health Workforce Accelerator: In Colorado and Georgia, our Mental Health Workforce Accelerator program helps students and recent graduates with job placement, salary support, and options for clinical supervision. This program focuses on placing workers at sites that serve vulnerable communities to help increase access to care.
To move beyond the mental health professional shortage, health care leaders and policymakers must think creatively and work together. The challenges we face as a country are significant and will only grow if we don’t address them now.
This challenge, however, is also an opportunity. Investing in the mental health workforce is not just about filling positions. It’s about creating meaningful job opportunities that serve a crucial role in our communities. These are exactly the kinds of investments the government and health care organizations should be looking to make. They provide purposeful work and address a vital community need.
By building on emerging programs, making strategic investments, and fostering collaboration, our country can transform this period of need into an era of wellness — one that benefits millions of Americans.