Our nation’s health suffers if Congress cuts Medicaid
Reducing Medicaid funding will lead to worse health outcomes, overburden emergency rooms, and cause many rural hospitals to close.
Medicaid helps millions of Americans stay healthier by providing care and coverage.
Medicaid gives millions of Americans access to the front door of the health care system. It helps keep them healthy and provides for those with acute and chronic care needs. And it is critical to the stability of providers and hospitals — especially rural hospitals.
Now Congress is debating Medicaid proposals that put both patients and the health care system at risk.
We urge policymakers to take a judicious approach to prevent changes that would harm the health of millions and undermine our health care system.
Medicaid ensures access to care
For almost 60 years, Medicaid has provided coverage and access to care for people with low incomes and people with disabilities, including 14 million Americans living in rural areas and 10 million Americans under the age of 65 who have disabilities.
Medicaid covers prenatal care, primary care, community-based preventive care, hospital services, and mental health care. It is the largest payer for nursing home care, and provides coverage and care for nearly 60% of children in the U.S.
Medicaid also covers substance use disorder treatment, covering close to 40% of Americans with opioid use disorder.
In 2014, many states expanded Medicaid eligibility with increased federal matching funds. Medicaid has always been funded with both state and federal dollars.
Today, only 8% of Americans are uninsured, a remarkable improvement since the days when 1 in every 5 Americans was uninsured.
Not only did this expansion cut the rate of non-elderly uninsured adults by more than half, it also improved health and reduced mortality.
Medicaid stabilizes America’s health care system
Medicaid plays an especially important role in supporting the financial integrity of community health centers and hospitals. Medicaid has been particularly critical for rural hospitals, providing financial stability at a time when almost 700 rural hospitals are at risk of closing.
Medicaid also helps community health centers augment and improve the care they offer. In states that expanded Medicaid, community health centers are more likely to offer medication-assisted treatment for opioid addiction.
For hospitals across the United States, Medicaid expansion has reduced their share of uncompensated care — that is, care for uninsured people without another source of payment.
Uncompensated care is a major financial burden on hospitals and other providers. Medicaid expansion has reduced uncompensated care by about 40%.
Medicaid and Kaiser Permanente
As part of Kaiser Permanente’s commitment to the communities we serve, we care for 1.5 million people who are insured through Medicaid.
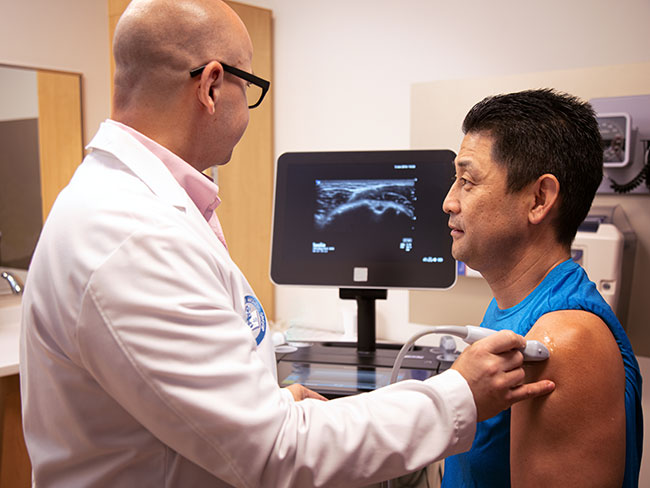
We take a population health approach to managing the care of our Medicaid members, proactively identifying their needs and risks to provide early and ongoing intervention.
We help members with a whole-person care approach — addressing their physical, mental, and social health needs. For example, we might help secure nutritious food and reliable transportation for a patient with diabetes who has struggled to eat a healthy diet and attend doctor appointments.
In addition to providing evidence-based care for diabetes, this approach is essential to preventing the costly long-term complications of uncontrolled risk factors, like high blood sugar.
This approach not only helps make each Medicaid member healthier, but it supports how we’re tackling the chronic disease epidemic for all our members.
The consequences of cuts and changes to eligibility
Congress is considering proposals that could change Medicaid financing and eligibility.
Some of these proposed changes could cause millions of people to lose access to care under Medicaid. People without coverage often skip necessary care, leading to worse health outcomes. For people in poor health, the results can be dangerous.
Cuts will put a greater burden on emergency rooms and community health providers.
Each additional uninsured person results in $900 in uncompensated health care costs. Hospitals absorb most of these costs. Ultimately, this means fewer services, higher prices, and reduced investments in their local community.
Federal cuts to Medicaid funding could also have a ripple effect in many states that have “trigger laws” that automatically reduce Medicaid care and coverage if federal matching funds are cut.
Policy recommendations
As Congress considers policy changes, new proposals should preserve care and coverage and the financial integrity of our health care system.
We urge lawmakers to support:
- Retaining the current share of federal funding for Medicaid — This is especially critical at a time when state budgets are tight, and many states are considering raising taxes to make up shortfalls
- Continued coverage for low-income adults receiving care and coverage from Medicaid expansion — This not only ensures care for these adults, it also helps community health centers and hospitals maintain financial stability
- A whole-person care approach — Policy leaders can bolster beneficiaries’ physical, mental, and social health by supporting Medicaid alongside other programs that help meet their social needs like housing, food security, education, and employment training
- Medicaid payment methodologies that account for the full range of health plan and provider models — This includes Kaiser Permanente’s integrated care model
If work requirements are imposed, policymakers should encourage support for social services and supports that minimize barriers to employment for low-income populations, including access to job training and employment programs, child care, transportation, mental health and wellness services, and substance use disorder treatment.
Finally, policymakers must understand the critical role that value-based care plays in ensuring access to care and in improving care quality in a manner that is financially sustainable for Medicaid. With competition among different care and coverage models on the basis of value, Medicaid and the people it serves will experience higher-quality and more-affordable care.
In the end, cutting federal funding doesn’t really save money — it just shifts costs elsewhere. Policymakers must pursue responsible solutions that preserve needed care.