How to prevent cervical cancer
Cervical cancer is highly preventable. HPV vaccination and regular screenings can greatly reduce your risk.
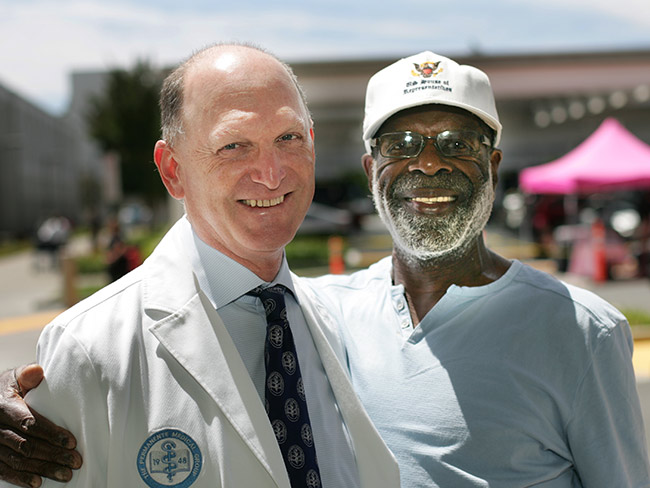
Our goal at Kaiser Permanente is to eliminate cervical cancer among our members and patients.
Cervical cancer was once a leading cause of cancer death for women in the United States.
Rates have decreased greatly over the past 20 years, thanks to improved prevention.
But we can do even better: Our goal is to end cervical cancer among our members.
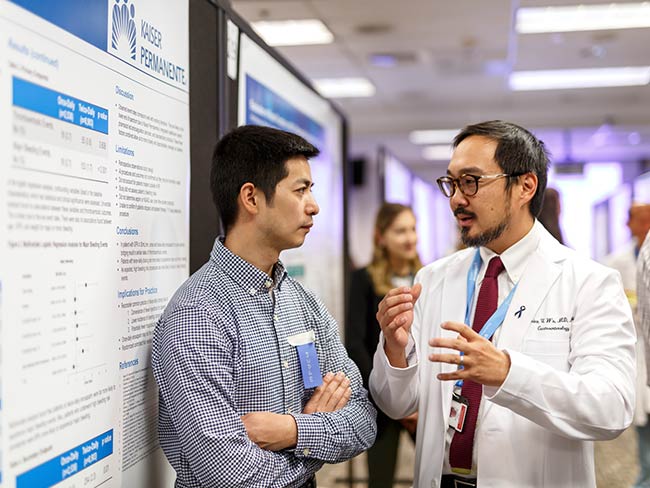
“Cervical cancer is completely preventable,” said Tracy Seo, MD, a Kaiser Permanente ob-gyn in Northern California. “Our 3-part strategy includes vaccination, screening, and timely treatment.”
Kaiser Permanente is a leader in cervical cancer prevention, with screening and vaccination rates in the top 10% nationwide.
Source: 2024 HEDIS® (Healthcare Effectiveness Data and Information Set)
Step 1: Vaccination
Almost all cervical cancers are caused by human papillomavirus, known as HPV.
HPV is common. Nearly everyone will get HPV at some point in their lives. In most cases, the body’s immune system clears the virus before cell changes develop. But when that doesn’t happen, HPV can lead to cancer.
Fortunately, there’s a simple way to prevent HPV: Get vaccinated.
- HPV vaccination works best as part of routine childhood vaccinations so young people are protected before they’re exposed to the virus.
- The HPV vaccine series is routinely recommended for adolescents at 11 or 12 years of age, but it may be started at age 9.
- We recommend that everyone get vaccinated before age 27.
If you’ve screened positive for HPV, vaccination may still benefit you. It could improve your immune response and help protect against other types of HPV.
“The HPV vaccine doesn’t just prevent cervical cancer,” Dr. Seo said. “It also helps prevent cancer of the vulva, vagina, penis, anus, and throat. So, it’s really a cancer prevention vaccine.”
Nearly 61% of eligible Kaiser Permanente members got vaccinated for HPV in 2023. That’s nearly twice the national average of 33%.
Source: 2024 HEDIS® (Healthcare Effectiveness Data and Information Set)
Step 2: Screening
The HPV vaccine provides long-lasting protection, but it doesn’t protect against all types of HPV. And it doesn’t prevent all forms of cervical cancer.
That’s why regular cervical cancer screening is essential. It helps detect warning signs before they become a problem. Cervical cancer can usually be treated successfully when it’s found early.
The best test for you depends on your age and prior test results. Doctors usually recommend a Pap test for people age 21 to 24 and an HPV test for people age 25 and older.
Talk with your doctor about how often you should be tested.
Kaiser Permanente’s cervical cancer screening rate of 82% exceeds the national average of 73%.
Source: 2024 HEDIS® (Healthcare Effectiveness Data and Information Set)
Step 3: Timely treatment
If your HPV test shows that HPV is present, or if your Pap test comes back as abnormal or unclear, it doesn’t mean you have cancer.
Your care team will work with you to develop a follow-up plan with recommendations based on your age, test results, and other factors.
“When people have access to the care they need, including vaccination and screening, their chances of getting cervical cancer are significantly reduced,” Dr. Seo said. “Our goal is to help people access the care they deserve.”
Learn more about cancer prevention at Kaiser Permanente.

May 7, 2025
How to cope with anxiety after childbirth
As a new mother, Cherissa Ong was overwhelmed by stress. A mental health …

March 27, 2025
Living proof: Colon cancer highly treatable if caught early
There is an alarming rise in colon cancer rates among younger adults. Cynthia …

February 26, 2025
Colon cancer: Do you need to be screened?
If you’re age 45 or older, getting checked regularly for colorectal cancer …

February 14, 2025
A fulfilling life on the other side of ovarian cancer
As a wife and a mother, Autumn Gray was determined to beat cancer to be …

February 12, 2025
Back on track after a rare cancer diagnosis
After facing sarcoma at age 18, drag-racing champion Cooper Chun needed …

January 24, 2025
Is one drink a day OK? Here’s what to consider
NPR

December 26, 2024
How telehealth can make life easier for people with cancer
Virtual care connects cancer patients like Rob Tufel to a wide range of …
November 18, 2024
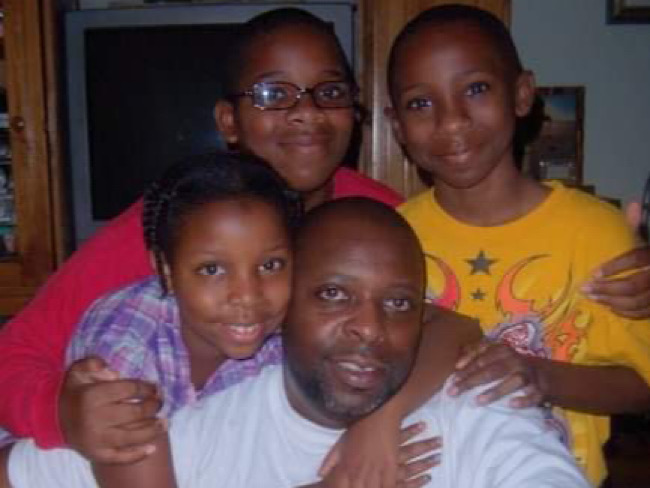
The power of early detection and proactive men’s health
A father's determination to stay healthy for his 3 children led him to …

October 1, 2024
Screening for breast cancer: Mammogram guidelines
A Kaiser Permanente radiologist answers commonly asked questions.
September 20, 2024
Ovarian cancer journey confirmed nursing student's calling
Miriam Gutierrez was diagnosed with late-stage ovarian cancer at age 31. …

September 18, 2024
Cancer rates are rising in younger age groups
‘Connect’ with research to help understand more about the increase of certain …

August 29, 2024
After Stage 4 ovarian cancer, she’s still going strong
Donna Budway received prompt surgery followed by chemotherapy. She credits …

August 26, 2024
Katie's ride: Motorcycle rally a surprise for patient
Kaiser Permanente in San Diego helped plan a special send-off for Katie …

June 17, 2024
That’s a lot of babies!
Delivering multiple babies is difficult, but Kaiser Permanente care teams …

June 17, 2024
A culture of caring eases a cancer journey
Exceptional, personalized radiation oncology care helped Maura Craig treat …

June 13, 2024
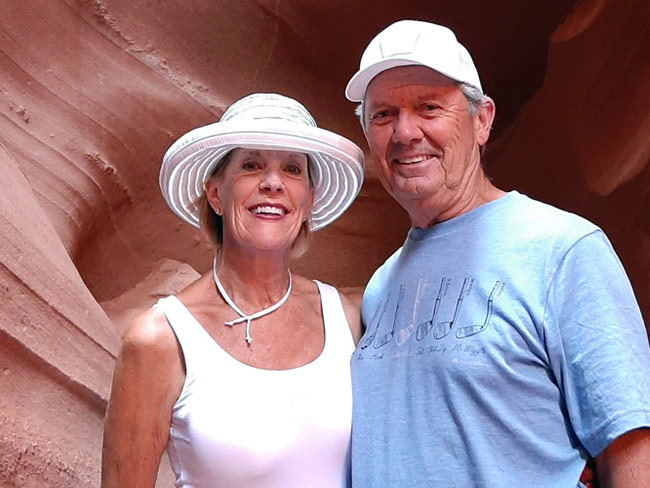
Conquered 2 cancers while climbing mountains
Chris Hogan faced kidney cancer and prostate cancer at the same time. He …

June 3, 2024
A call to ‘Connect’ for cancer prevention research
Participate in a study to help uncover the causes of cancer and how to …

May 31, 2024
Stage 4 lung cancer: A story of hope
A young father is enjoying “bonus time” with his kids thanks to new targeted …

May 21, 2024
Surviving stage 4 lung cancer with immunotherapy treatment
Patients like Carol Pitman are living longer thanks to advances in lung …

May 7, 2024
Making cancer care more convenient in Southern California
Kaiser Permanente has opened a new Radiation Oncology Center at the Bellflower …

April 17, 2024
5 common health conditions men don’t like to talk about
Some of the most common conditions affecting men carry a social stigma …

April 1, 2024
Lynch syndrome: Managing the risk of hereditary colon cancer
Lynch syndrome is a gene mutation that increases colon cancer risk. Learn …
March 20, 2024
Life after cancer: Surviving and thriving
A healthy life after cancer is possible. Learn how Kaiser Permanente helps …

March 14, 2024
Midwife offers personal care for mom facing complications
For Sam Beeson, having a midwife at her side during her pregnancy helped …

March 6, 2024
Joining a national effort to test new ways to find cancer
As part of the Cancer Screening Research Network, our researchers will …

March 6, 2024
Colon cancer screening: She’s glad she didn’t wait
A timely preventive test reveals Rebecca Kucera has cancer. Swift treatment …
March 5, 2024
Researchers look for ways to find pancreatic cancer early
Early detection of the disease, before it becomes advanced, will increase …

February 21, 2024
Recovering at home after a double mastectomy
Innovative surgical recovery program helps breast cancer patients safely …

February 7, 2024
To stay well, get vaccinated and practice healthy habits
Cases of flu, COVID-19, and RSV continue to spread in our communities. …

February 1, 2024
Take a break from cannabis while expecting, study suggests
Research shows that marijuana use during pregnancy increases health risks …

January 24, 2024
A full-circle journey for one cancer survivor
Grateful for compassionate and successful Hodgkin lymphoma treatment at …

January 10, 2024
‘You don’t know unless you ask them’
Kaiser Permanente’s Patient Advisory Councils help us create exceptional …

December 21, 2023
It’s not too late to get your flu shot
Flu season often continues into early spring. Here are 5 reasons you should …

December 13, 2023
Nurse navigators guide patients from diagnosis to treatment
An unexpected cancer diagnosis left Jennifer Martin unsure of the next …

December 6, 2023
Leading research with gratitude
Learn how you can participate in a study to uncover what causes cancer …

December 6, 2023
Video prenatal visits are a boon for a busy working mom
A new care option offers a mix of in-person and virtual visits, supported …

December 1, 2023
Surviving — and thriving — after cancer
From diagnosis to recovery, David Parsons, MD, shares how screening, treatment, …

October 25, 2023
Breast cancer during pregnancy: Caring for mom and baby
A team of specialists treats an expecting mother’s cancer while keeping …

October 23, 2023
A renewed sense of purpose after surviving breast cancer
Joy Short, a Kaiser Permanente member and employee, turned her breast cancer …

October 17, 2023
Flu protection for all that is you
Getting vaccinated is a safe and effective way to avoid getting sick.

October 11, 2023
Early breast cancer detection improves quality of life
For 75-year-old Peggy Dickston, a surprise diagnosis was caught early thanks …

October 10, 2023
What to know about COVID-19 vaccines
The updated vaccine is recommended for everyone 6 months and older.

August 29, 2023
Preventing overdoses starts with education
Risk factors are not always associated with addiction or substance abuse. …

August 17, 2023
Beyond clinic walls: Research supporting healthy communities
Stories in the Department of Research & Evaluation 2022 Annual Report demonstrat …

August 17, 2023
Cancer research: The role of immunotherapy
Research and clinical trials play a vital role in advancing cancer treatment …

August 16, 2023
Cervical cancer screening: Exploring the at-home HPV test
Kaiser Permanente is at the forefront of cervical cancer research. Find …

August 15, 2023
'Hot-spot' strategy gets more Californians vaccinated
A new location-based vaccine strategy by Kaiser Permanente was successful …

August 14, 2023
Marla’s story: Surviving acute promyelocytic leukemia
After a diagnosis for a rare type of blood cancer, Marla Marriott got high-quali …
August 4, 2023
Eating well and adopting healthy habits helps prevent cancer
Learn how lifestyle medicine is part of cancer care at Kaiser Permanente.

July 27, 2023
Courageously facing hereditary breast cancer
Fay Gordon's breast cancer was caught in the early stages thanks to genetic …

July 26, 2023
Can you get chemotherapy while pregnant?
Chemotherapy can be an option during pregnancy. Find out how Kaiser Permanente …

July 21, 2023
Thankful for every day after HPV-related cancer diagnosis
Michael West shares his incredible journey from diagnosis to treatment …

July 14, 2023
Breast reconstruction surgery after cancer
A Kaiser Permanente plastic surgeon explains breast reconstruction options …

July 11, 2023
We deliver excellence for parents and babies
Our members are more likely to feed their babies breast milk. And they’re …

July 10, 2023
Beating colon cancer together: Miguel and Paula’s story
After they were both diagnosed with colon cancer, Miguel and Paula fought …

June 30, 2023
Doctors' top tips to manage prostate cancer risk factors
Regardless of your age, race, or family history, you can take steps to …

June 30, 2023
Lung cancer survivor received ‘pioneering’ care
Doctor and mother of 3 Susan Brim received top-notch care after her lung …

June 27, 2023
Comforting, personalized care for a kiddo with cancer
Carter Shaver from Portland, Oregon, shares his optimistic smile after …

June 22, 2023
Higher survival rates for our patients with colon cancer
A new study compares Kaiser Permanente members in Southern California to …

June 21, 2023
And that’s why they call postpartum the blues
Take time to adjust to a new baby and lifestyle changes — and reach out …

June 15, 2023
Stay safe while having fun in the sun
Tips for preventing sunburn and decreasing the risk of skin cancer.

June 14, 2023
Living with stage 4 breast cancer
Thanks to personalized care from a team of skilled doctors, Christina McAmis …

May 30, 2023
The healing power of shared cancer experience
Peer mentoring program matches new cancer patients with others who’ve gone …

April 25, 2023
Hannah Peters, MD, provides essential care to ‘Rosies’
When thousands of women industrial workers, often called “Rosies,” joined …

April 14, 2023
The importance of screening for gestational diabetes
Gestational diabetes poses a significant risk to women of color, particularly …

April 12, 2023
Having her ‘rainbow baby’ after a high-risk pregnancy
Remote perinatal monitoring and frequent in-person appointments helped …

March 17, 2023
A call to 'Connect' for cancer research
A new study invites participants in Oregon to help uncover what causes …

March 14, 2023
Colorectal cancer on the rise among younger adults
Learn why early screening is crucial for prevention and treatment.

March 13, 2023
Making waves with our first female sports ambassador
Kaiser Permanente in Southern California partners with San Diego Wave Fútbol …

February 28, 2023
What you need to know about COPD
Almost 16 million people in the United States have chronic obstructive …

February 28, 2023
A conversation about pregnancy and women’s heart health
New research shows blood pressure patterns early in pregnancy can identify …

February 27, 2023
Teaching flu a lesson
School-based flu vaccination clinics made it safe and convenient for students …

February 24, 2023
Nurturing expectant moms who have substance use disorders
Project Nurture in Portland, Oregon, provides treatment and a path forward …

February 15, 2023
A new chapter for male patient with breast cancer
A multidisciplinary care team acted fast to help save the life of a Kaiser …

January 27, 2023
Timely flu vaccinations at community events
Proactive flu prevention outreach helped community members in Downey, California …

January 13, 2023
Making dreams come true
Member achieves bucket list goal of helping to build a Rose Parade float, …

December 21, 2022
From cancer patient to cancer colleague
A Kaiser Permanente member’s cancer journey inspires her to join the team …

November 14, 2022
It’s time to rethink health care quality measurement
To meaningfully improve health equity, we must shift our focus to outcomes …

September 27, 2022
Maternity appointments from the comfort of home
New care option offers pregnant patients a mix of in-person and video visits.

August 17, 2022
Cancer clinical trials: Can they help find a cure?
These important research studies aim to help patients live longer, better …

August 3, 2022
When breastfeeding is a struggle, you can help
By lending a hand with dinners, diapers, and dishes, you can give loved …

August 3, 2022
Supporting new moms in the postpartum period
By reaching out early and providing care that’s personalized to parents’ …

June 27, 2022
Kids 6 months to 17 years can receive COVID-19 vaccination
Providing safe and effective vaccinations to children is an important step …

May 12, 2022
Endometriosis and motherhood: Grace’s story
She wanted relief from pain and a healthy baby. Her care team delivered.

May 5, 2022
Research study will inform the future of cancer prevention
Connect for Cancer Prevention Study’s goal to recruit 200,000 participants …

April 20, 2022
The perfect match: Living kidney donation saves LAPD officer
Bobbie Norman is grateful for 15 years of health after his wife — a fellow …

December 6, 2021
Faith leaders use trusted voices to encourage vaccination
Grants expand support for faith-based organizations working to protect …

November 30, 2021
Bechara Choucair, MD, returns as chief health officer
After serving on the White House COVID-19 response team, Bechara Choucair, …
October 12, 2021
Beyond advocacy: Requiring vaccination to stop COVID-19
Kaiser Permanente and other leading companies are mandating COVID-19 shots …

October 1, 2021
Our support of California’s student vaccination requirement
A statement from Kaiser Permanente chair and chief executive officer Greg …

June 8, 2021
Cancer patients and physicians embrace telehealth
Video visits and virtual collaboration speed cancer care transformation …

April 28, 2021
COVID-19 outcomes are more severe for people of color
Kaiser Permanente research underscores the importance of culturally appropriate …
April 5, 2021
Weight linked to risk of second cancer after breast cancer
Kaiser Permanente study has important public health implications given …

March 23, 2021
Vaccine Equity Toolkit will help address equitable access
As vaccines bring hope to end the pandemic, Kaiser Permanente’s toolkit …

March 11, 2021
Our support of the American Rescue Plan Act
A statement from CEO Greg A. Adams about the American Rescue Plan Act.

July 21, 2020
Diagnostic and preventive care is in our DNA
A routine screening helped detect Bill Walsh’s cancer before it became …

January 21, 2020
Destination health: Stopping cancer before it starts
Kaiser Permanente is creating more healthy life years with a combined focus …

March 6, 2013
Decades of health records fuel Kaiser Permanente research
Over 50 years of early Kaiser Permanente electronic health records since …