Supporting new moms in the postpartum period
By reaching out early and providing care that’s personalized to parents’ needs, Kaiser Permanente helps ease a time of intense change.
Marivic Uytengsu and her baby, Angelique.
After a difficult pregnancy, Marivic Uytengsu was excited and relieved to give birth to a healthy baby girl in March 2021 at Kaiser Permanente Antioch Medical Center in Northern California.
Uytengsu had struggled with nausea and vomiting throughout her first trimester, twice needing intravenous fluids for dehydration. In her third trimester, she developed pain and numbness in her hands from carpal tunnel syndrome, a common issue in pregnancy.
The 30-year-old was looking forward to bonding with her daughter, Angelique. But there were more challenges ahead. Still coping with carpal tunnel syndrome, Uytengsu struggled to position the baby for breastfeeding.
“I wanted to breastfeed because I know it’s healthy for the baby, but she couldn’t latch on, and it was really hard,” she said. “We were home alone all day, and we were both struggling. When she would cry, I would cry.”
Uytengsu soon developed mastitis, an infection that can be caused by not fully emptying the breast, and noticed that her milk supply was decreasing.
Postpartum challenges
Difficulty getting started with breastfeeding is one of many challenges parents may face in the 3 months after the birth of a child, a period sometimes referred to as the “fourth trimester.” It’s a time of intense physical, social, and emotional change.
“Even if you had a relatively easy birth, you’re dealing with physical changes as your body recovers,” said Kari Carlson, MD, chair of obstetrics and gynecology and director of women’s health for Kaiser Permanente in Northern California. “You’re also going through the transition of bringing a new baby home. Add to that the worries and stresses all parents experience, plus sleep deprivation, and it can be a difficult time.”
We were home alone all day, and we were both struggling. When she would cry, I would cry. Marivic Uytengsu
Recognizing how challenging the fourth trimester can be, the American College of Obstetricians and Gynecologists in 2018 published new guidance on postpartum care, redefining it as “an ongoing process, rather than a single encounter, with services and support tailored to each woman’s individual needs.” The guidance recommends that women have contact with their care providers within 3 weeks after birth and a comprehensive postpartum visit by 12 weeks.
Meeting moms and babies where they are
At Kaiser Permanente, efforts to better meet the needs of moms and newborns were already underway. In 2017, Kaiser Permanente pioneered a “couplet care” model in Hawaii, combining postpartum checkups for mom and baby.
“We were already seeing newborns 1 to 3 days after they left the hospital,” explained Mabel Wong, MD, chief of obstetrics and gynecology. “But most moms weren’t being seen for 4 weeks. Since most moms were bringing their babies to the first appointment, we decided that was an ideal time to check in on mom as well as baby.”
Today, moms and babies are seen at the Mom Newborn Center on Oahu 1 to 3 days after discharge. Women are checked for high blood pressure, a leading cause of maternal death in the postpartum period. People who’ve had cesarean sections receive wound care. Certified lactation consultants help with breastfeeding.
The visit also includes a mental health and wellness assessment.
“The fourth trimester is a stressful time, so if there’s a risk of intimate partner violence, postpartum depression, or other struggles, that’s often when we see it,” Dr. Wong said.
When concerns are identified, clinicians at the Mom Newborn Center can seamlessly connect patients to higher-level care.
Care that meets mom’s needs
In Colorado and Georgia, Kaiser Permanente has used home visits to support new families. Maternal child health nurses travel to the patient’s home to examine mom and baby, help with breastfeeding, and address social and emotional concerns.
And in Northern California, Kaiser Permanente uses a range of tools to keep in close contact with new moms — from post-discharge follow-up calls and emails to video and phone visits.
“Many of our moms tell us they prefer video visits, because they don’t have to pack up the baby or worry about exposure to COVID-19,” Dr. Carlson said. “For our clinicians, a video visit is a great way to get a more complete picture of how parents are doing because they can see their interactions with the baby and the rest of the family.”
Timely advice
For Uytengsu, a secure email exchange with a pediatrician and certified lactation consultant was the turning point in her troubles. The doctor encouraged her to use a breast pump to maintain and increase her milk supply — and to feed the milk to Angelique in a bottle.
Once her carpal tunnel syndrome improved, Uytengsu was able to get her baby to latch on using a breastfeeding position that the physician taught her. It didn’t take long before Angelique was breastfeeding exclusively.
“I’m very happy and proud of myself for sticking with it,” said Uytengsu.
Find tips on the first few weeks at home with a new baby.
-
Social Share
- Share Supporting New Moms in the Postpartum Period on Pinterest
- Share Supporting New Moms in the Postpartum Period on LinkedIn
- Share Supporting New Moms in the Postpartum Period on Twitter
- Share Supporting New Moms in the Postpartum Period on Facebook
- Print Supporting New Moms in the Postpartum Period
- Email Supporting New Moms in the Postpartum Period

May 22, 2025
Los Angeles area wildfires: How we helped our communities
We moved quickly to ensure that people in our communities could still get …

May 19, 2025
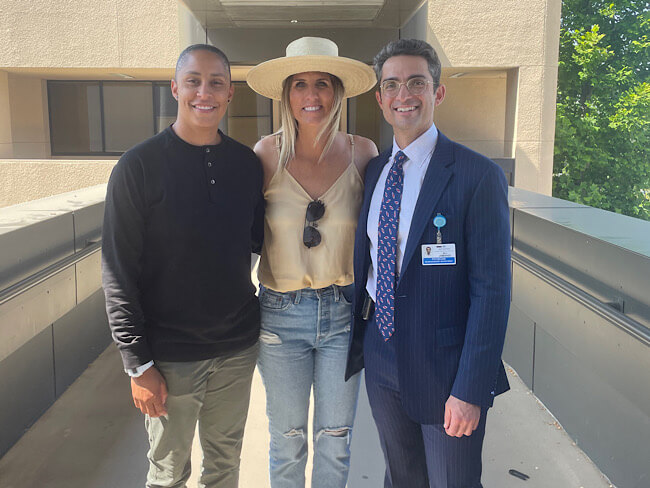
A champion for healthy motherhood
As an Olympic athlete, Shannon Rowbury fought for better maternity policies. …

May 19, 2025
Member praises 50 years of collaboration with care teams
Karen Hansen’s doctors and clinicians have partnered with her to customize …

May 7, 2025
How to cope with anxiety after childbirth
As a new mother, Cherissa Ong was overwhelmed by stress. A mental health …

May 6, 2025
Best maternity hospitals: We have 29 of them
Our high-quality, compassionate care landed us on Newsweek’s 2025 list …

April 30, 2025
From fighter to father: How addiction care changed his life
Travis Taylor has substance use disorder and mental health conditions. …

April 23, 2025
Healing the human spirit
Kaiser Permanente strives to support survivors of sexual violence.

March 29, 2025
We are meeting mental health care access requirements
The investments we’ve made over the last several years have resulted in …

March 27, 2025
Living proof: Colon cancer highly treatable if caught early
There is an alarming rise in colon cancer rates among younger adults. Cynthia …

March 27, 2025
We’re committed to mentorship, mental health, and communities
Kaiser Permanente awarded Elevate Your G.A.M.E. a grant to expand program …

March 7, 2025
High blood pressure during pregnancy is on the rise
The keys to preventing cardiovascular conditions during pregnancy are knowing …

March 7, 2025
Kaiser Permanente in Hawaii cures 1,000th patient with hepatitis C
The milestone highlights its Viral Hepatitis Clinic's crucial role in addressing …

February 27, 2025
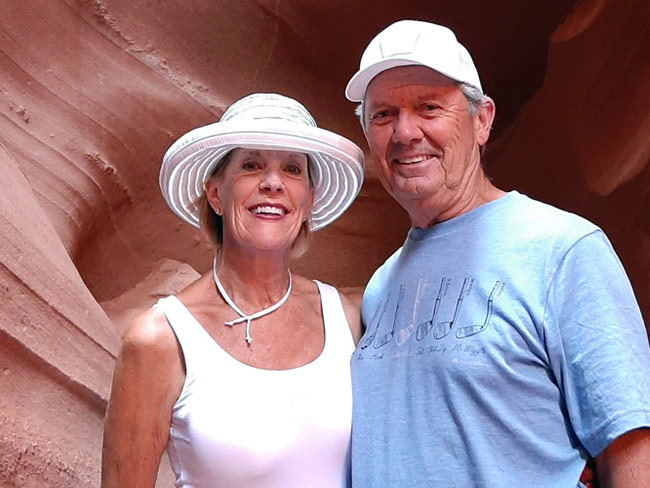
‘The heart attack that saved my life’
A sudden heart attack led Mark Twichel to seek care at Kaiser Permanente …

February 26, 2025
Colon cancer: Do you need to be screened?
If you’re age 45 or older, getting checked regularly for colorectal cancer …

February 26, 2025
Spring into a better night’s sleep
A Kaiser Permanente sleep expert shares tips for decreasing the impact …

February 25, 2025
Providing care to trauma survivors
Kaiser Permanente has been at the forefront of recognizing how trauma impacts …

February 18, 2025
I just need a chance
Billy Cardosi spent his life putting his family and job first. Then a heart-rela …

February 14, 2025
A fulfilling life on the other side of ovarian cancer
As a wife and a mother, Autumn Gray was determined to beat cancer to be …

February 11, 2025
Stressed about the news? Try a ‘news diet’ — and hugs
When news and online information become too stressful, Dr. Sammie LaMont …

February 4, 2025
What is therapy, anyway?
At Kaiser Permanente, our care is personalized for each patient's mental …

January 24, 2025
Is one drink a day OK? Here’s what to consider
NPR

January 22, 2025
A preteen overcomes anxiety and suicidal thoughts
A young Kaiser Permanente member speaks up to gain the mental health support …

January 15, 2025
After surgery, home was where his heart was
Virtual cardiac rehabilitation offers Mike Erskine a convenient, safe way …

January 13, 2025
How to prevent cervical cancer
Cervical cancer is highly preventable. HPV vaccination and regular screenings …

December 26, 2024
How telehealth can make life easier for people with cancer
Virtual care connects cancer patients like Rob Tufel to a wide range of …

December 19, 2024
From darkness to sobriety and recovery
Once suicidal and on the verge of losing his job, Eric Jeffers has found …

December 13, 2024
How to stay happy and healthy over the holidays
Sammie LaMont Moss, MD, a psychiatrist for Kaiser Permanente in Colorado, …

December 10, 2024
Accelerating growth in the mental health care workforce
Actions policymakers can take to grow and diversify the mental health care …

November 26, 2024
How to reduce your risk of stroke
A Kaiser Permanente doctor and researcher shares the simple changes you …
November 18, 2024
The power of early detection and proactive men’s health
A father's determination to stay healthy for his 3 children led him to …

November 13, 2024
Self-care for caregivers matters: Here’s why
A sharp increase in rates of adult caregiving is taking a mental and physical …

November 12, 2024
Surviving lung cancer as a nonsmoker
As a lifelong nonsmoker, Mariann Stephens was shocked to learn she had …

November 4, 2024
Recruitment and retention in behavioral health
An expert’s insights on the changing mental health landscape, its impact …
October 29, 2024
That’s not tennis elbow
A Kaiser Permanente physician thought he pinched a nerve during a tennis …

October 23, 2024
Doomscrolling? It may affect your heart.
Endless bad news is just one fingertip away online. One Kaiser Permanente …

October 15, 2024
107-year-old member credits Kaiser Permanente for longevity
Bettye Garrett’s personal doctor says her healthy perspective on life’s …

October 10, 2024
Child anxiety relief: Therapy gets a digital boost
Shiloh Sevin’s well-being improves thanks to her psychologist and the Calm …

October 8, 2024
Exploring your relationship with alcohol
If you're rethinking your habits, here are some questions to keep in mind.

October 8, 2024
It started with a bad feeling
In August 2023, John Lynn collapsed at work. For the next year, he fought …

October 4, 2024
Study shows new way to prevent suicides
Primary care teams can make a big difference in their patients’ lives, …

October 4, 2024
Teacher learns about herself and how to live with anxiety
A lifelong educator seeks behavioral health care to manage repetitive worries, …

October 1, 2024
Screening for breast cancer: Mammogram guidelines
A Kaiser Permanente radiologist answers commonly asked questions.
October 1, 2024
From depression to connection: Older adult finds her way
After a long period of loneliness and isolation, Roberta Maguire gets the …

September 27, 2024
Youth suicide in the digital age is raising concerns
Young people face growing pressures from social media, school, and other …

September 27, 2024
Traumatized children find mental health therapy beneficial
A Ventura County community-based nonprofit provides counselors to help …
September 20, 2024
Ovarian cancer journey confirmed nursing student's calling
Miriam Gutierrez was diagnosed with late-stage ovarian cancer at age 31. …

September 18, 2024
More than 100 ‘Top Docs’ recognized in Washington state
Kaiser Permanente celebrates doctors and nurse practitioners recognized …

September 17, 2024
A Latina’s voice in mental health is impactful with her clients
Connecting through a shared heritage gives one therapist a unique perspective …

September 17, 2024
Playing on after 2 decades of cancer care
With the support of his health care team and nurse navigator, musician …

September 17, 2024
Groundbreaking at new medical offices in Pueblo
The new Pueblo North Medical Offices will replace the existing facility …

September 11, 2024
Buprenorphine saves lives. Why can’t more patients get it?
Policy changes are crucial for better opioid addiction treatment.

September 6, 2024
Navigating a world turned upside down after heart failure
After a life-threatening series of heart attacks at age 57, Bunnell Fockler …

August 29, 2024
After Stage 4 ovarian cancer, she’s still going strong
Donna Budway received prompt surgery followed by chemotherapy. She credits …
August 29, 2024
Neurosurgery and a deep, enduring doctor-patient relationship
A basketball coach’s remarkable story of undergoing brain tumor surgery …

August 28, 2024
Making breastfeeding work: A second-time mom’s journey
Support from a dedicated care team helps Tiffany Anonye breastfeed her …

August 27, 2024
From sore throats to ice cream floats
A mother and daughter share a special bond after undergoing tonsillectomies …

August 16, 2024
After severe depression, a ‘rainbow lit up my sky’
Shannon Parkin survived 7 suicide attempts. She shares her story of hope …

August 15, 2024
Back home one day after heart surgery
Ed Dalmasso needed an aortic valve replacement. His care team provided …

August 6, 2024
For a father with prostate cancer, knowledge is power
Harold Newman had advanced prostate cancer. Genetic testing helped expand …

August 1, 2024
Kaiser Permanente tops Colorado ‘Top Doctors’ list
5280 Magazine named 332 Kaiser Permanente physicians to its annual Top …

July 11, 2024
Expecting parents find community and support in group visits
Maureen McLoughlin’s experience with care in a group setting gave her the …

July 11, 2024
Transforming education and mental health in Watts
Our investment in the Watts neighborhood of California, in partnership …

July 10, 2024
We help members lower their risk of heart attacks and strokes
A Southern California program, powered by our connected care model, is …

July 2, 2024
Best maternity hospitals: We have 29 of them
Our safe, high-quality, compassionate care landed us on Newsweek’s America’s …

June 28, 2024
Health Action Summit highlights mental health opportunities
The Kaiser Permanente Colorado Health Action Summit gathered nonprofits, …

June 27, 2024
5 facts about autism
A Kaiser Permanente doctor shares key details. By learning more about autism, …

June 25, 2024
Prompt postpartum care saves a baby’s life
When a newborn was diagnosed with meningitis, a life-threatening infection …

June 19, 2024
Investments in Black community promote total health for all
Funding from Kaiser Permanente in Washington helps to promote mental health, …

June 17, 2024
That’s a lot of babies!
Delivering multiple babies is difficult, but Kaiser Permanente care teams …

June 13, 2024
Conquered 2 cancers while climbing mountains
Chris Hogan faced kidney cancer and prostate cancer at the same time. He …

May 31, 2024
Stage 4 lung cancer: A story of hope
A young father is enjoying “bonus time” with his kids thanks to new targeted …

May 21, 2024
Surviving stage 4 lung cancer with immunotherapy treatment
Patients like Carol Pitman are living longer thanks to advances in lung …

May 14, 2024
A key ally in navigating mental health care for kids
Behavioral health consultants can provide a better understanding of often …

May 10, 2024
Self-care is key for new parents
Feeling emotional or overwhelmed after a new baby’s arrival? You’re not …

May 3, 2024
Lonely and depressed — but not alone
After a lifetime of feeling isolated, Moth Wygal finds connection thanks …
May 1, 2024
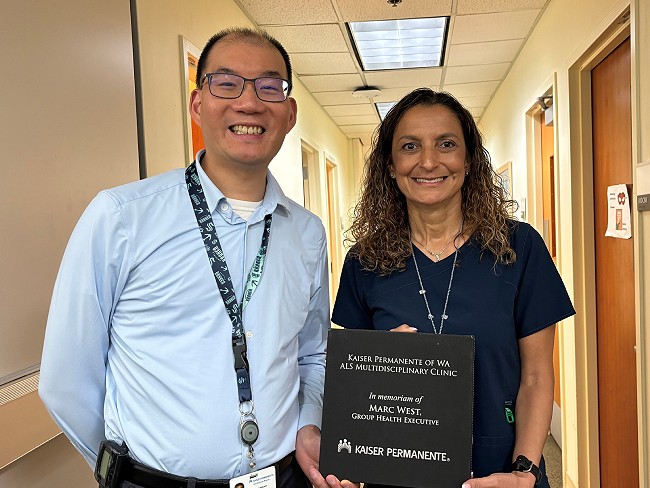
Tacoma ALS clinic recognized for high-quality care
Patients with amyotrophic lateral sclerosis, also called Lou Gehrig’s disease, …
April 29, 2024
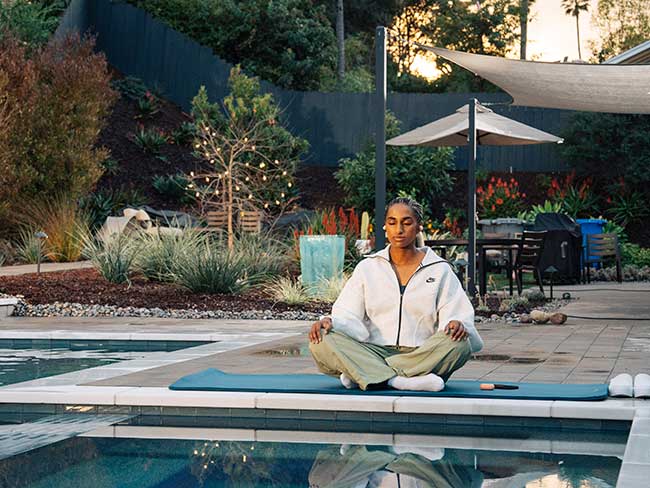
Soccer star: ‘Let’s talk about mental health’
Naomi Girma, a sports ambassador for Kaiser Permanente, is passionate about …

April 12, 2024
It’s time to address America’s Black maternal health crisis
Health care leaders and policymakers should each play their part to help …

April 10, 2024
For a new mom, talking about her worries helped her heal
One in 5 people experience depression, anxiety, or other mental health …

April 9, 2024
Denver Fire Department annual blood work screenings triple
It’s easy to put off recommended health screenings, and sometimes even …

April 8, 2024
Reducing inequity with fruits and vegetables
Black Americans experience worse health outcomes compared to other populations. …

April 1, 2024
Lynch syndrome: Managing the risk of hereditary colon cancer
Lynch syndrome is a gene mutation that increases colon cancer risk. Learn …

March 29, 2024
Faster recovery: From cardiac scare to exploring Italy
Virtual cardiac rehab helped Mike Kelly heal at home after a life-threatening …
March 20, 2024
Life after cancer: Surviving and thriving
A healthy life after cancer is possible. Learn how Kaiser Permanente helps …

March 14, 2024
Healthy kidneys support overall good health
Kaiser Permanente excels in preventing, detecting, and treating kidney …

March 14, 2024
Midwife offers personal care for mom facing complications
For Sam Beeson, having a midwife at her side during her pregnancy helped …
March 5, 2024
Researchers look for ways to find pancreatic cancer early
Early detection of the disease, before it becomes advanced, will increase …
February 22, 2024
The journey of a lifetime
Care teams at Kaiser Permanente Fontana Medical Center helped Phillip Crawford …

February 21, 2024
From planning his funeral to celebrating his wedding
Gabriel Abarca had no hope for his future. Then the team at Kaiser Permanente …

February 21, 2024
Recovering at home after a double mastectomy
Innovative surgical recovery program helps breast cancer patients safely …

February 13, 2024
A legacy of life-changing community support and partnership
The Kaiser Permanente Watts Counseling and Learning Center started as a …

February 12, 2024
Proposition 1 would bolster mental health care in California
Kaiser Permanente supports the ballot measure to expand and improve mental …

February 2, 2024
Expanding medical, social, and educational services in Watts
Kaiser Permanente opens medical offices and a new home for the Watts Counseling …

February 1, 2024
Take a break from cannabis while expecting, study suggests
Research shows that marijuana use during pregnancy increases health risks …

January 29, 2024
Empowering minds to help others thrive
Supporting behavioral and mental health in communities where needs are …

January 24, 2024
A full-circle journey for one cancer survivor
Grateful for compassionate and successful Hodgkin lymphoma treatment at …

January 22, 2024
Solutions for strengthening the mental health care workforce
Better public policies can help address the challenges. We encourage policymaker …

January 17, 2024
How diabetes can affect your heart
People with diabetes are more likely to have heart disease.

January 10, 2024
‘You don’t know unless you ask them’
Kaiser Permanente’s Patient Advisory Councils help us create exceptional …

January 3, 2024
Addressing the shortage of mental health workers
There aren’t enough mental health professionals in the U.S. to meet the …