The healing language of cancer
A Kaiser Permanente radiation oncologist shares how giving patients a voice on how we talk about their illness can provide comfort and healing.
Sometimes, when we talk to patients who have cancer, we say the wrong thing, over and over and over. We tell them they’re in the midst of a battle, or a war. We tell them they can beat it if they fight it, if they’re strong, if they never give up.
But what if all the pain, suffering, and indignity they’ve endured in chemotherapy has left them wanting to close their eyes and rest peacefully in the knowledge that their time has come? Urging them to fight is not going to make them feel better. It might make them feel worse — as if they did not try hard enough and failed.
“There’s better healing language that can be used,” says Katie Deming, MD. “But it’s going to be different for everyone.”
Giving the patient a voice
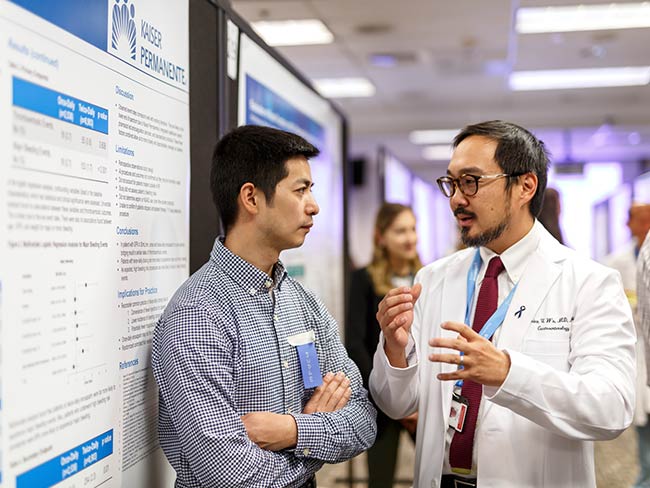
Dr. Deming is a radiation oncologist and former medical director of cancer services for Kaiser Permanente in Portland, Oregon. She wants to change the way we talk to patients with cancer. Specifically, she wants to give the patients a voice in how we discuss their illness. She recently gave a TEDx talk in Reno, Nevada, titled How to Talk to Someone With Cancer.
About a decade ago, Dr. Deming and her colleagues surveyed 1,400 patients who had breast cancer to share their feelings about the term “cancer survivor.” She wasn’t prepared for the results: 60% of the respondents considered the term “survivor” to be negative. Patients said it didn’t accurately reflect their unique experience of cancer. Others felt as if they were tempting fate to say they’d “survived.” Some expressed anger, saying they had stage 4 cancer and that survival wasn’t likely.
“This made me really pay attention to the language I used,” Dr. Deming said recently. “And when I started looking more closely, I realized we tend to use a lot of battle language, like ‘Win the fight.’ I also noticed that these terms were not helping my patients.”
Emotionally charged language
When it comes to cancer, most of us rely on language that suggests “fighting” means it can be “beaten,” a comforting sentiment that puts off unpleasant thoughts about death and provides a sense that the illness is temporary and soon everything will be back to normal.
But it can mean something else entirely for the patient. Some may feel compelled to give chemotherapy or other treatments another try because they don’t want to “give up the fight” and disappoint their family when they’d really rather accept their mortality and die on their own terms. Using the language of the battlefield doesn’t motivate these patients. In fact, in some cases it may increase cortisol levels and anxiety and weaken the immune system. Rather than being calming and supportive, this language could aggravate their suffering.
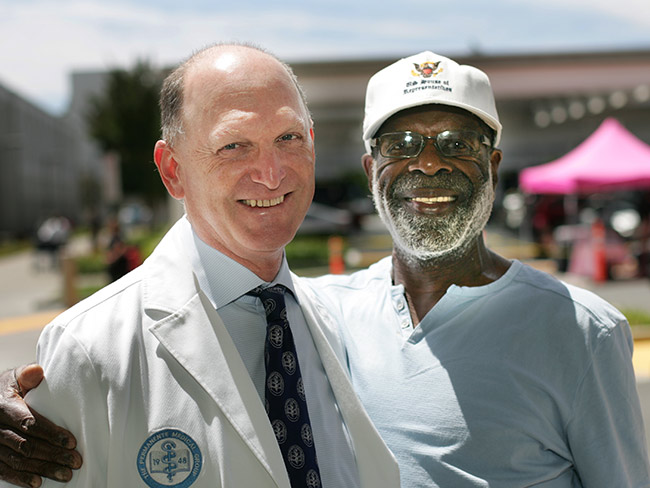
So, Deming is trying to start a different conversation and it starts by putting the patients’ needs first. And to find out what exactly the patient needs, the best start is to ask them.
“It’s ok to say, ‘I want you to know I’m here for you and I want to know what’s most supportive for you.’”
When Dr. Deming asked a close family member with breast cancer how she could be most supportive, her relative said she loved to see photos of house pets. So, rather than daily texts that put the onus on the patient – How are you? – Dr. Deming sent along photos of her pets.
They were a big hit — which isn’t surprising. Laughing at a cat chasing its own tail is a nice respite from “fighting for your life.”

July 11, 2024
Transforming education and mental health in Watts
Our investment in the Watts neighborhood of California, in partnership …

June 28, 2024
Health Action Summit highlights mental health opportunities
The Kaiser Permanente Colorado Health Action Summit gathered nonprofits, …

June 27, 2024
5 facts about autism
A Kaiser Permanente doctor shares key details. By learning more about autism, …

June 19, 2024
Investments in Black community promote total health for all
Funding from Kaiser Permanente in Washington helps to promote mental health, …

June 17, 2024
A culture of caring eases a cancer journey
Exceptional, personalized radiation oncology care helped Maura Craig treat …

June 13, 2024
Conquered 2 cancers while climbing mountains
Chris Hogan faced kidney cancer and prostate cancer at the same time. He …

June 3, 2024
A call to ‘Connect’ for cancer prevention research
Participate in a study to help uncover the causes of cancer and how to …

May 31, 2024
Stage 4 lung cancer: A story of hope
A young father is enjoying “bonus time” with his kids thanks to new targeted …

May 21, 2024
Surviving stage 4 lung cancer with immunotherapy treatment
Patients like Carol Pitman are living longer thanks to advances in lung …

May 14, 2024
A key ally in navigating mental health care for kids
Behavioral health consultants can provide a better understanding of often …

May 10, 2024
Self-care is key for new parents
Feeling emotional or overwhelmed after a new baby’s arrival? You’re not …

May 7, 2024
Making cancer care more convenient in Southern California
Kaiser Permanente has opened a new Radiation Oncology Center at the Bellflower …

May 3, 2024
Lonely and depressed — but not alone
After a lifetime of feeling isolated, Moth Wygal finds connection thanks …
April 29, 2024
Soccer star: ‘Let’s talk about mental health’
Naomi Girma, a sports ambassador for Kaiser Permanente, is passionate about …

April 17, 2024
5 common health conditions men don’t like to talk about
Some of the most common conditions affecting men carry a social stigma …

April 10, 2024
For a new mom, talking about her worries helped her heal
One in 5 people experience depression, anxiety, or other mental health …

April 1, 2024
Lynch syndrome: Managing the risk of hereditary colon cancer
Lynch syndrome is a gene mutation that increases colon cancer risk. Learn …
March 20, 2024
Life after cancer: Surviving and thriving
A healthy life after cancer is possible. Learn how Kaiser Permanente helps …

March 6, 2024
Joining a national effort to test new ways to find cancer
As part of the Cancer Screening Research Network, our researchers will …

March 6, 2024
Colon cancer screening: She’s glad she didn’t wait
A timely preventive test reveals Rebecca Kucera has cancer. Swift treatment …
March 5, 2024
Researchers look for ways to find pancreatic cancer early
Early detection of the disease, before it becomes advanced, will increase …

February 26, 2024
What you need to know about colon cancer screenings
Screening for colorectal cancer is recommended for most people starting …

February 21, 2024
From planning his funeral to celebrating his wedding
Gabriel Abarca had no hope for his future. Then the team at Kaiser Permanente …

February 21, 2024
Recovering at home after a double mastectomy
Innovative surgical recovery program helps breast cancer patients safely …

February 13, 2024
A legacy of life-changing community support and partnership
The Kaiser Permanente Watts Counseling and Learning Center started as a …

February 12, 2024
Proposition 1 would bolster mental health care in California
Kaiser Permanente supports the ballot measure to expand and improve mental …

February 8, 2024
Road to heart health: Living well
You have only one heart. ‘Prescribe’ yourself a few changes to help protect …

February 2, 2024
Expanding medical, social, and educational services in Watts
Kaiser Permanente opens medical offices and a new home for the Watts Counselin …

January 29, 2024
Empowering minds to help others thrive
Supporting behavioral and mental health in communities where needs are …

January 24, 2024
A full-circle journey for one cancer survivor
Grateful for compassionate and successful Hodgkin lymphoma treatment at …

January 23, 2024
How to bolster your child’s self-esteem
Everyday Health

January 22, 2024
Solutions for strengthening the mental health care workforce
Better public policies can help address the challenges. We encourage policymak …

January 10, 2024
‘You don’t know unless you ask them’
Kaiser Permanente’s Patient Advisory Councils help us create exceptional …

January 3, 2024
Addressing the shortage of mental health workers
There aren’t enough mental health professionals in the U.S. to meet the …

December 26, 2023
How to prevent cervical cancer
Cervical cancer is highly preventable. Learn how HPV vaccination and regular …

December 13, 2023
Nurse navigators guide patients from diagnosis to treatment
An unexpected cancer diagnosis left Jennifer Martin unsure of the next …

December 7, 2023
Safe, secure housing is a must for health
We offer housing-related legal help to prevent evictions and remove barriers …

December 6, 2023
Leading research with gratitude
Learn how you can participate in a study to uncover what causes cancer …

December 1, 2023
Surviving — and thriving — after cancer
From diagnosis to recovery, David Parsons, MD, shares how screening, treatment …

November 29, 2023
Tapping into an array of mental health options
Pavan Somusetty, MD, explains how people who need support and guidance …

November 21, 2023
Surviving lung cancer as a nonsmoker
As a lifelong nonsmoker, Mariann Stephens was shocked to learn she had …

November 1, 2023
Tips for healthy holiday travel
Six steps help you prep for winter trips.

October 25, 2023
Breast cancer during pregnancy: Caring for mom and baby
A team of specialists treats an expecting mother’s cancer while keeping …

October 24, 2023
Childhood anxiety: What parents need to know
A child and adolescent psychiatrist shares tips on supporting your child …

October 23, 2023
A renewed sense of purpose after surviving breast cancer
Joy Short, a Kaiser Permanente member and employee, turned her breast cancer …

October 11, 2023
Early breast cancer detection improves quality of life
For 75-year-old Peggy Dickston, a surprise diagnosis was caught early thanks …

October 11, 2023
Bridging the mental health gap
Kaiser Permanente’s partnership with Fontana Unified School District brings …

September 27, 2023
Harvest your power
Use biofeedback to help manage stress.

September 27, 2023
From suicide survivor to mental health advocate
Former Major League Baseball player Drew Robinson shares his story of hope …

September 13, 2023
Mental health champion: A mission inspired by personal loss
San Diego Wave Fútbol Club star defender Naomi Girma, Kaiser Permanente …

September 6, 2023
Recovery from addiction is possible
Our clinicians help patients get the care they need to move forward with …

August 28, 2023
Grants improve the total health of our communities
Kaiser Permanente increases access to mental health services in Southern …

August 22, 2023
Mental health
Expanding access to high-quality mental health services

August 17, 2023
Beyond clinic walls: Research supporting healthy communities
Stories in the Department of Research & Evaluation 2022 Annual Report demonstr …

August 17, 2023
Cancer research: The role of immunotherapy
Research and clinical trials play a vital role in advancing cancer treatment …

August 16, 2023
Cervical cancer screening: Exploring the at-home HPV test
Kaiser Permanente is at the forefront of cervical cancer research. Find …

August 15, 2023
Screening for breast cancer: Mammogram guidelines
Mammograms can help detect breast cancer early, when it’s easier to treat. …

August 14, 2023
Marla’s story: Surviving acute promyelocytic leukemia
After a diagnosis for a rare type of blood cancer, Marla Marriott got high-qua …

August 10, 2023
Successfully navigating the school year
These tips from Don Mordecai, MD, Kaiser Permanente’s national mental health …

August 8, 2023
Genetic testing and customized cancer care
Harold Newman had advanced prostate cancer. Genetic testing helped expand …
August 4, 2023
Eating well and adopting healthy habits helps prevent cancer
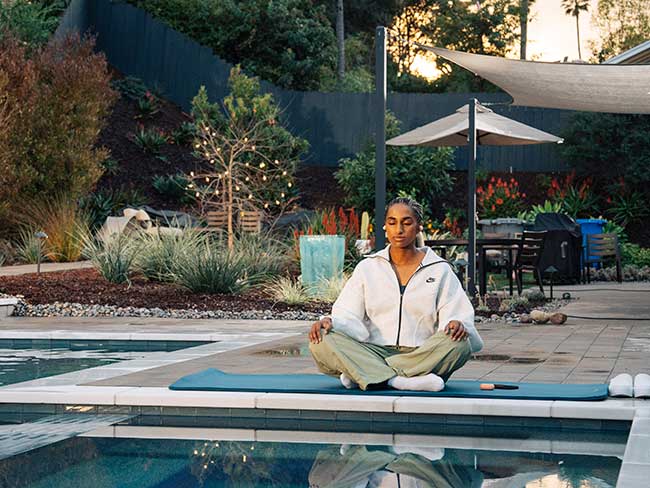
Learn how lifestyle medicine is part of cancer care at Kaiser Permanente.

July 27, 2023
Courageously facing hereditary breast cancer
Fay Gordon's breast cancer was caught in the early stages thanks to genetic …

July 26, 2023
Can you get chemotherapy while pregnant?
Chemotherapy can be an option during pregnancy. Find out how Kaiser Permanente …

July 21, 2023
Thankful for every day after HPV-related cancer diagnosis
Michael West shares his incredible journey from diagnosis to treatment …

July 14, 2023
Breast reconstruction surgery after cancer
A Kaiser Permanente plastic surgeon explains breast reconstruction options …

July 11, 2023
Cancer care for the body, mind, and spirit
Many people with cancer experience depression and anxiety. Mental health …

July 10, 2023
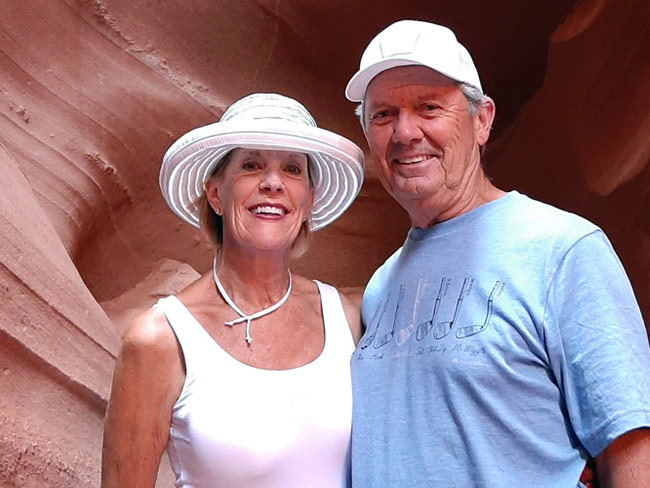
Beating colon cancer together: Miguel and Paula’s story
After they were both diagnosed with colon cancer, Miguel and Paula fought …

June 30, 2023
Men's mental well-being is a priority
Unique challenges and societal pressures can impact men’s emotional well-being …

June 30, 2023
Doctors' top tips to manage prostate cancer risk factors
Age, family history, and race are key factors.

June 30, 2023
Lung cancer survivor received ‘pioneering’ care
Doctor and mother of 3 Susan Brim received top-notch care after her lung …

June 28, 2023
Making waves to empower young girls
Kaiser Permanente and the San Diego Wave Fútbol Club host a second Wave …

June 27, 2023
Comforting, personalized care for a kiddo with cancer
Carter Shaver from Portland, Oregon, shares his optimistic smile after …

June 23, 2023
Get the mental health support you need
Kaiser Permanente is here to help with care and valuable tools to support …

June 22, 2023
Employee joined Connect study after bloodwork results
Help change the future of cancer prevention by joining Connect today.

June 22, 2023
Higher survival rates for our patients with colon cancer
A new study compares Kaiser Permanente members in Southern California to …

June 21, 2023
And that’s why they call postpartum the blues
Take time to adjust to a new baby and lifestyle changes — and reach out …

June 15, 2023
Stay safe while having fun in the sun
Tips for preventing sunburn and decreasing the risk of skin cancer.

June 14, 2023
Living with stage 4 breast cancer
Thanks to personalized care from a team of skilled doctors, Christina McAmis …

June 9, 2023
Mental health, addiction, and the power of a peer
Shared experience helps young people in Oregon build confidence for their …

June 7, 2023
Teen social media use may lead to depression
Creating a healthy relationship with social media can help safeguard the …

June 5, 2023
Understanding and living with bipolar disorder
A Kaiser Permanente member shares his personal journey of navigating bipolar …

June 1, 2023
Policy recommendations from a mental health therapist in training
Changing my career and becoming a therapist revealed ways our country can …

May 30, 2023
The healing power of shared cancer experience
Peer mentoring program matches new cancer patients with others who’ve gone …

May 22, 2023
Sidelined by injury, a former nurse seeks depression care
Susan Sandhu struggled to find meaning in her life after an injury forced …

May 18, 2023
Addressing mental health trauma in a local community
Trauma-informed outreach efforts in Orange County are being recognized …

May 16, 2023
Managing trauma does not need to be traumatic
Expanded access to high-quality, affordable mental health care supports …
May 9, 2023
School shootings provoke anxiety in many children
Child psychiatrist defines anxiety, its symptoms, how to address it, and …

May 4, 2023
An unexpected cancer diagnosis
As a nonsmoker, Betty Schuldt’s stage 4 lung cancer diagnosis was surprising, …

April 25, 2023
Hannah Peters, MD, provides essential care to ‘Rosies’
When thousands of women industrial workers, often called “Rosies,” joined …

March 29, 2023
Volunteering helps create healthier communities
Kaiser Permanente’s partnership with Special Olympics Southern California …

March 24, 2023
Finding hope after a mental health and addiction crisis
Treatment for bipolar disorder and opiate addiction helps a Kaiser Permanente …

March 17, 2023
A call to 'Connect' for cancer research
A new study invites participants in Oregon to help uncover what causes …

March 16, 2023
Supporting our children after acts of mass violence
Southern California psychiatrist offers practical advice for parents to …

March 14, 2023
Colorectal cancer on the rise among younger adults
Learn why early screening is crucial for prevention and treatment.

March 13, 2023
Making waves with our first female sports ambassador
Kaiser Permanente in Southern California partners with San Diego Wave Fútbol …

March 7, 2023
For moments when you may not need to see a therapist
Kaiser Permanente provides members with convenient ways to improve their …

March 1, 2023
Spring forward: How to prepare for losing an hour of sleep
A sleep expert shares 4 practical tips for coping with the time shift and …

February 24, 2023
Nurturing expectant moms who have substance use disorders
Project Nurture in Portland, Oregon, provides treatment and a path forward …

February 23, 2023
Eating disorders on the rise among teens
Expert shares 5 valuable tips for parents and guardians to help children …

February 15, 2023
A new chapter for male patient with breast cancer
A multidisciplinary care team acted fast to help save the life of a Kaiser …