Weight linked to risk of second cancer after breast cancer
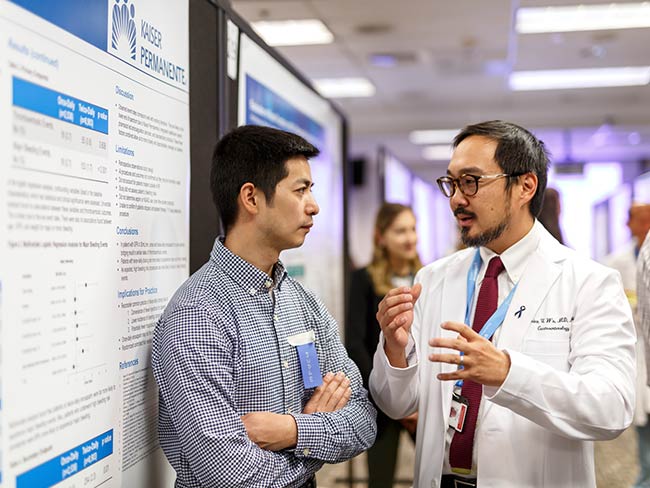
Kaiser Permanente study has important public health implications given the number of breast cancer survivors with excess body weight.
PRESS RELEASE
Contact: Elizabeth Whitehead
elizabeth.m.whitehead@kp.org
720-910-3016
Kerry Sinclair
ksinclair@webershandwick.com
310-854-8278
DENVER — Breast cancer survivors who are overweight have a statistically significant increased risk of developing second primary cancers, according to results from a study conducted by Kaiser Permanente researchers and published in the Journal of the National Cancer Institute.
There are approximately 3.9 million breast cancer survivors in the United States today and studies have found women diagnosed with breast cancer have an 18% increased risk for developing a second cancer compared to the general population. This increased risk is likely due to shared risk factors between the first and second cancers, genetic susceptibility, and long-term effects of breast cancer treatment.
Obesity is also strongly associated with an increased risk of several types of cancer. In fact, an estimated 55% of all cancers in women occur in those who are overweight or obese. This study sought to examine the association between body weight, as measured by BMI, at initial breast cancer diagnosis and the risk of developing a second cancer among a large cohort of women diagnosed with invasive breast cancer.
Women diagnosed with an invasive breast cancer were at a small but statistically significant increased risk for second cancers associated with increasing BMI. The association was more pronounced when the analysis was limited to cancers that are “obesity-related,” or for second breast cancers, and was strongest for a diagnosis of estrogen receptor-positive second breast cancer. This study was the first to examine the risk of a subsequent ER-positive breast cancer or obesity-related cancers specifically.
“These findings have important public health implications given the number of breast cancer survivors with excess body weight,” said lead author Heather Spencer Feigelson, PhD, senior investigator at the Kaiser Permanente Colorado Institute for Health Research. “Our study examined whether cancer survivors are at an increased risk of developing a second cancer and what factors contribute to this increased risk. Our findings truly underscore the need for effective weight loss prevention strategies, including nutrition and physical activity guidelines for breast cancer survivors.”
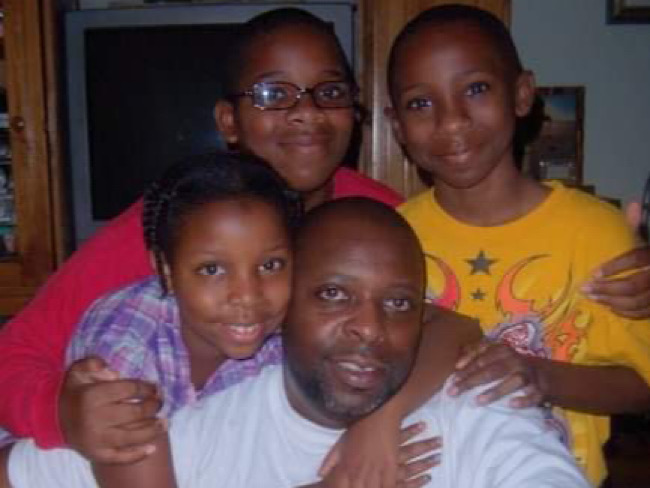
This study involved 6,481 women from Kaiser Permanente in Colorado and Washington, of whom 822 (12.7%) developed a second cancer. The majority of women were overweight (33.4%) or obese (33.8%) at the time of their initial diagnosis. The mean age at initial breast cancer diagnosis was 61 years, and most (82.2%) of the cohort was white. Black women comprised a small percentage of the cases but were more likely to be obese (50.9% of Black women were obese compared to 33.6% of white women). The patients’ BMI at the first cancer was extracted from their medical records. The outcomes evaluated included: all second cancers, obesity-related second cancers, any second breast cancer, and ER-positive second breast cancers. Obesity related cancer includes colorectal, uterine, ovarian and pancreatic cancer.
“This study illustrates that modifying one’s BMI may result in significant health and quality of life benefits among breast cancer survivors,” explained Clara Bodelon, PhD, MS, Division of Cancer Epidemiology and Genetics at the National Cancer Institute, part of the National Institutes of Health.
The study was funded by the Intramural Research Program of the Division of Cancer Epidemiology and Genetics of the National Cancer Institute, in addition to contracts to Kaiser Permanente in Colorado from the National Cancer Institute. Kaiser Permanente in Washington was supported by grants and contracts from the American Cancer Society and the National Cancer Institute.
Authors on the study include Clara Bodelon, PhD, MS, Division of Cancer Epidemiology and Genetics, National Cancer Institute, Bethesda, Maryland; J. David Powers, MS, Kaiser Permanente Colorado Institute for Health Research, Denver, Colorado; Rochelle E. Curtis, MA, Division of Cancer Epidemiology and Genetics, National Cancer Institute; Diana S.M. Buist, PhD, MPH, Kaiser Permanente Washington Health Research Institute, Seattle, Washington; Lene H.S.Veiga, PhD, Division of Cancer Epidemiology and Genetics, National Cancer Institute; Erin J. Aiello Bowles, MPH, Kaiser Permanente Washington Health Research Institute; Amy Berrington de Gonzalez, DPhil, Division of Cancer Epidemiology and Genetics, National Cancer Institute; and Gretchen L Gierach, PhD, MPH, Division of Cancer Epidemiology and Genetics, National Cancer Institute.
Since 2007, Kaiser Permanente scientists have published over 500 articles related to breast cancer risk, prevention, diagnosis, treatment, and post-treatment monitoring.
About Kaiser Permanente
Kaiser Permanente is committed to helping shape the future of health care. We are recognized as one of America’s leading health care providers and not-for-profit health plans. Founded in 1945, Kaiser Permanente has a mission to provide high-quality, affordable health care services and to improve the health of our members and the communities we serve. We currently serve 12.4 million members in 8 states and the District of Columbia. Care for members and patients is focused on their total health and guided by their personal Permanente Medical Group physicians, specialists, and team of caregivers. Our expert and caring medical teams are empowered and supported by industry-leading technology advances and tools for health promotion, disease prevention, state-of-the-art care delivery, and world-class chronic disease management. Kaiser Permanente is dedicated to care innovations, clinical research, health education, and the support of community health.