Study of mental health treatment trends early in pandemic
Analysis compared outpatient contacts between March 9 and May 31, 2020.
PRESS RELEASE
Contacts: Jan Greene
janice.x.greene@kp.org
510-504-2663
Kerry Sinclair
ksinclair@webershandwick.com
310-854-8278
OAKLAND, Calif. — A detailed analysis of mental health treatment trends during the COVID-19 pandemic found a 7% increase in visits during the initial shelter-in-place period in 2020, compared with the same 3-month period in 2019.
The study, published in The Journal of Clinical Psychiatry March 3, examined patient visits for psychiatric diagnoses among members of Kaiser Permanente in Northern California.
The greatest increases in visits were for substance use (up 51%), adjustment disorder (up 15%), anxiety (up 12%), bipolar disorder (up 9%), and psychotic disorder (up 6%). Adjustment disorder is diagnosed when someone responds to a stressful life event with symptoms such as sadness and hopelessness.
“The increases we found in patients seeking care for substance use and anxiety are consistent with other data showing the pandemic and shelter-in-place orders were difficult for many people,” said lead author Kathryn Erickson-Ridout, MD, PhD, a psychiatrist with Kaiser Permanente in Northern California and a member of the Physician Researcher Program with the Kaiser Permanente Northern California Division of Research. “These findings reflect what I experienced with my patients who sought out care.”
The analysis focused on a period when Kaiser Permanente pivoted to virtual visits by video and telephone to ensure that patients continued to have access to care when shelter-in-place orders were implemented. “COVID-19 has created huge psychosocial disruption,” Dr. Erickson-Ridout said. “It’s impacting people’s ability to work, socialize, and have relationships, and that is having mental health consequences. We were able to respond to that with a robust telehealth system, to reach those patients and give them good care.”
The study was a retrospective observational analysis comparing 165,696 psychiatric outpatient contacts between March 9 and May 31, 2019, with 181,015 during the same period in 2020, an increase of 7%. The researchers also confirmed the shift away from in-person visits, tallying a 264% increase in telephone and video visits from the year before. Kaiser Permanente clinicians also offer mental health support by secure email message, but this study did not count those.
The study found 42% more addiction clinic visits than the same period in 2019. This could be related to patients having more difficulty coping with the pandemic, but it could also reflect existing patients having good connections with their addiction medicine providers, said study senior author Esti Iturralde, PhD, a research scientist with the Division of Research. “They may have been able to seek care more easily from the health system because of the strong connections and supports Kaiser Permanente provides, including case management,” she said.
The results also suggest some people did not immediately adjust to the new virtual visit format. Visits with new patients declined by 42%, as did visits by children and adolescents (down 23%), and older adults (down more than 5%).
The authors said these results may reflect which patients were most comfortable reaching out for telehealth care, at least during the first few months of the pandemic. Reliance on caregivers to facilitate visits, or healthcare avoidance during this time, may be behind these changes. Future research may reflect how patients adjusted to virtual visits past May 2020.
To increase use of virtual visits by these groups, and people with new mental health symptoms, the authors suggested outreach through collaborative care, such as getting referrals from primary care providers and other clinicians patients see for physical health concerns.
The research was supported by The Permanente Medical Group Delivery Science and Applied Research Initiative and Physician Researcher Program.
Other coauthors were Constance Weisner, DrPH, MSW, Cynthia Campbell, PhD, MPH, and Mubarika Alavi, MS, of the Division of Research; Samuel J. Ridout, MD, PhD, Maria T. Koshy, MD, Inderpreet Dhillon, MD, and Sameer Awsare, MD, of The Permanente Medical Group; and Brooke Harris, PhD, of the Kaiser Permanente Oakland Medical Center.
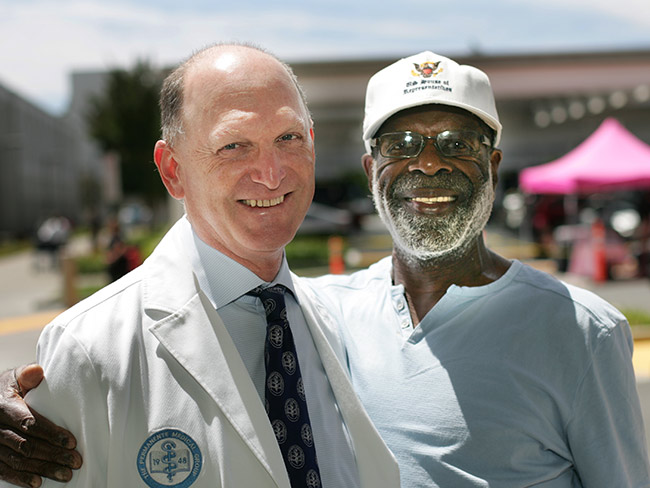
About Kaiser Permanente
Kaiser Permanente is committed to helping shape the future of health care. We are recognized as one of America’s leading health care providers and not-for-profit health plans. Founded in 1945, Kaiser Permanente has a mission to provide high-quality, affordable health care services and to improve the health of our members and the communities we serve. We currently serve 12.4 million members in 8 states and the District of Columbia. Care for members and patients is focused on their total health and guided by their personal Permanente Medical Group physicians, specialists, and team of caregivers. Our expert and caring medical teams are empowered and supported by industry-leading technology advances and tools for health promotion, disease prevention, state-of-the-art care delivery, and world-class chronic disease management. Kaiser Permanente is dedicated to care innovations, clinical research, health education, and the support of community health.
-
Social Share
- Share Study of Mental Health Treatment Trends Early in Pandemic on Pinterest
- Share Study of Mental Health Treatment Trends Early in Pandemic on LinkedIn
- Share Study of Mental Health Treatment Trends Early in Pandemic on Twitter
- Share Study of Mental Health Treatment Trends Early in Pandemic on Facebook
- Print Study of Mental Health Treatment Trends Early in Pandemic
- Email Study of Mental Health Treatment Trends Early in Pandemic

May 7, 2025
How to cope with anxiety after childbirth
As a new mother, Cherissa Ong was overwhelmed by stress. A mental health …

April 30, 2025
From fighter to father: How addiction care changed his life
Travis Taylor has substance use disorder and mental health conditions. …

April 23, 2025
Healing the human spirit
Kaiser Permanente strives to support survivors of sexual violence.

March 29, 2025
We are meeting mental health care access requirements
The investments we’ve made over the last several years have resulted in …

March 27, 2025
We’re committed to mentorship, mental health, and communities
Kaiser Permanente awarded Elevate Your G.A.M.E. a grant to expand program …

February 26, 2025
Spring into a better night’s sleep
A Kaiser Permanente sleep expert shares tips for decreasing the impact …

February 25, 2025
Providing care to trauma survivors
Kaiser Permanente has been at the forefront of recognizing how trauma impacts …

February 11, 2025
Stressed about the news? Try a ‘news diet’ — and hugs
When news and online information become too stressful, Dr. Sammie LaMont …

February 4, 2025
What is therapy, anyway?
At Kaiser Permanente, our care is personalized for each patient's mental …

January 24, 2025
Is one drink a day OK? Here’s what to consider
NPR

January 22, 2025
A preteen overcomes anxiety and suicidal thoughts
A young Kaiser Permanente member speaks up to gain the mental health support …

December 19, 2024
From darkness to sobriety and recovery
Once suicidal and on the verge of losing his job, Eric Jeffers has found …

December 13, 2024
How to stay happy and healthy over the holidays
Sammie LaMont Moss, MD, a psychiatrist for Kaiser Permanente in Colorado, …

December 10, 2024
Accelerating growth in the mental health care workforce
Actions policymakers can take to grow and diversify the mental health care …

November 13, 2024
Self-care for caregivers matters: Here’s why
A sharp increase in rates of adult caregiving is taking a mental and physical …

November 4, 2024
Recruitment and retention in behavioral health
An expert’s insights on the changing mental health landscape, its impact …

October 23, 2024
Doomscrolling? It may affect your heart.
Endless bad news is just one fingertip away online. One Kaiser Permanente …

October 10, 2024
Child anxiety relief: Therapy gets a digital boost
Shiloh Sevin’s well-being improves thanks to her psychologist and the Calm …

October 8, 2024
Exploring your relationship with alcohol
If you're rethinking your habits, here are some questions to keep in mind.

October 4, 2024
Study shows new way to prevent suicides
Primary care teams can make a big difference in their patients’ lives, …

October 4, 2024
Teacher learns about herself and how to live with anxiety
A lifelong educator seeks behavioral health care to manage repetitive worries, …
October 1, 2024
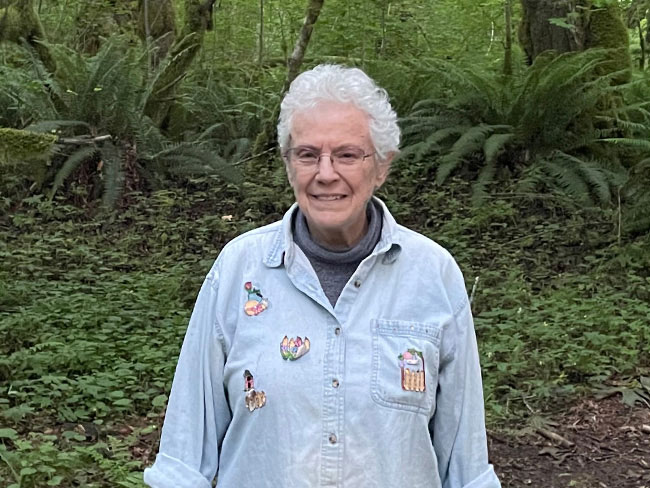
From depression to connection: Older adult finds her way
After a long period of loneliness and isolation, Roberta Maguire gets the …

September 27, 2024
Youth suicide in the digital age is raising concerns
Young people face growing pressures from social media, school, and other …

September 27, 2024
Traumatized children find mental health therapy beneficial
A Ventura County community-based nonprofit provides counselors to help …

September 17, 2024
A Latina’s voice in mental health is impactful with her clients
Connecting through a shared heritage gives one therapist a unique perspective …

September 11, 2024
Buprenorphine saves lives. Why can’t more patients get it?
Policy changes are crucial for better opioid addiction treatment.

August 16, 2024
After severe depression, a ‘rainbow lit up my sky’
Shannon Parkin survived 7 suicide attempts. She shares her story of hope …

July 11, 2024
Transforming education and mental health in Watts
Our investment in the Watts neighborhood of California, in partnership …

June 28, 2024
Health Action Summit highlights mental health opportunities
The Kaiser Permanente Colorado Health Action Summit gathered nonprofits, …

June 27, 2024
5 facts about autism
A Kaiser Permanente doctor shares key details. By learning more about autism, …

June 19, 2024
Investments in Black community promote total health for all
Funding from Kaiser Permanente in Washington helps to promote mental health, …

May 14, 2024
A key ally in navigating mental health care for kids
Behavioral health consultants can provide a better understanding of often …

May 10, 2024
Self-care is key for new parents
Feeling emotional or overwhelmed after a new baby’s arrival? You’re not …

May 3, 2024
Lonely and depressed — but not alone
After a lifetime of feeling isolated, Moth Wygal finds connection thanks …
April 29, 2024
Soccer star: ‘Let’s talk about mental health’
Naomi Girma, a sports ambassador for Kaiser Permanente, is passionate about …

April 10, 2024
For a new mom, talking about her worries helped her heal
One in 5 people experience depression, anxiety, or other mental health …

February 21, 2024
From planning his funeral to celebrating his wedding
Gabriel Abarca had no hope for his future. Then the team at Kaiser Permanente …

February 13, 2024
A legacy of life-changing community support and partnership
The Kaiser Permanente Watts Counseling and Learning Center started as a …

February 12, 2024
Proposition 1 would bolster mental health care in California
Kaiser Permanente supports the ballot measure to expand and improve mental …

February 2, 2024
Expanding medical, social, and educational services in Watts
Kaiser Permanente opens medical offices and a new home for the Watts Counseling …

January 29, 2024
Empowering minds to help others thrive
Supporting behavioral and mental health in communities where needs are …

January 24, 2024
A full-circle journey for one cancer survivor
Grateful for compassionate and successful Hodgkin lymphoma treatment at …

January 22, 2024
Solutions for strengthening the mental health care workforce
Better public policies can help address the challenges. We encourage policymaker …

January 3, 2024
Addressing the shortage of mental health workers
There aren’t enough mental health professionals in the U.S. to meet the …

December 7, 2023
Safe, secure housing is a must for health
We offer housing-related legal help to prevent evictions and remove barriers …

November 29, 2023
Tapping into an array of mental health options
Pavan Somusetty, MD, explains how people who need support and guidance …

October 24, 2023
Childhood anxiety: What parents need to know
A child and adolescent psychiatrist shares tips on supporting your child …

October 11, 2023
Bridging the mental health gap
Kaiser Permanente’s partnership with Fontana Unified School District brings …

September 27, 2023
Harvest your power
Use biofeedback to help manage stress.

September 27, 2023
From suicide survivor to mental health advocate
Former Major League Baseball player Drew Robinson shares his story of hope …

September 13, 2023
Mental health champion: A mission inspired by personal loss
San Diego Wave Fútbol Club star defender Naomi Girma, Kaiser Permanente …

September 6, 2023
Recovery from addiction is possible
Our clinicians help patients get the care they need to move forward with …

August 28, 2023
Grants improve the total health of our communities
Kaiser Permanente increases access to mental health services in Southern …

August 22, 2023
Mental health
Expanding access to high-quality mental health services

August 10, 2023
Successfully navigating the school year
These tips from Don Mordecai, MD, Kaiser Permanente’s national mental health …
August 4, 2023
Eating well and adopting healthy habits helps prevent cancer
Learn how lifestyle medicine is part of cancer care at Kaiser Permanente.

June 30, 2023
Men's mental well-being is a priority
Unique challenges and societal pressures can impact men’s emotional well-being.

June 28, 2023
Making waves to empower young girls
Kaiser Permanente and the San Diego Wave Fútbol Club host a second Wave …

June 23, 2023
Get the mental health support you need
Kaiser Permanente is here to help with care and valuable tools to support …

June 21, 2023
And that’s why they call postpartum the blues
Take time to adjust to a new baby and lifestyle changes — and reach out …

June 9, 2023
Mental health, addiction, and the power of a peer
Shared experience helps young people in Oregon build confidence for their …

June 7, 2023
Teen social media use may lead to depression
Creating a healthy relationship with social media can help safeguard the …

June 5, 2023
Understanding and living with bipolar disorder
A Kaiser Permanente member shares his personal journey of navigating bipolar …

June 1, 2023
Policy recommendations from a mental health therapist in training
Changing my career and becoming a therapist revealed ways our country can …

May 22, 2023
Sidelined by injury, a former nurse seeks depression care
Susan Sandhu struggled to find meaning in her life after an injury forced …

May 18, 2023
Addressing mental health trauma in a local community
Trauma-informed outreach efforts in Orange County are being recognized …

May 16, 2023
Managing trauma does not need to be traumatic
Expanded access to high-quality, affordable mental health care supports …
May 9, 2023
School shootings provoke anxiety in many children
Child psychiatrist defines anxiety, its symptoms, how to address it, and …

March 29, 2023
Volunteering helps create healthier communities
Kaiser Permanente’s partnership with Special Olympics Southern California …

March 24, 2023
Finding hope after a mental health and addiction crisis
Treatment for bipolar disorder and opiate addiction helps a Kaiser Permanente …

March 16, 2023
Supporting our children after acts of mass violence
Southern California psychiatrist offers practical advice for parents to …

March 13, 2023
Making waves with our first female sports ambassador
Kaiser Permanente in Southern California partners with San Diego Wave Fútbol …

March 7, 2023
For moments when you may not need to see a therapist
Kaiser Permanente provides members with convenient ways to improve their …

February 24, 2023
Nurturing expectant moms who have substance use disorders
Project Nurture in Portland, Oregon, provides treatment and a path forward …

February 23, 2023
Eating disorders on the rise among teens
Expert shares 5 valuable tips for parents and guardians to help children …

February 7, 2023
Employee honored for her dedication to our communities
Valerie Dionne wins our 2023 George Halvorson Community Health Leadership …

February 2, 2023
Addressing social isolation in the Northwest
Kaiser Permanente invests $3.3 million to build healthy social connections …

January 19, 2023
Understanding stress and how to manage it
A Kaiser Permanente psychiatrist shares advice for coping when stress won't …

November 14, 2022
It’s time to rethink health care quality measurement
To meaningfully improve health equity, we must shift our focus to outcomes …

September 7, 2022
How you can help prevent suicide
When someone you care about is struggling, it can be hard to know what …

August 29, 2022
For student athletes, mental wellness is a game changer
A sports medicine physician and mental health therapist discuss the mind-body …

August 3, 2022
Supporting new moms in the postpartum period
By reaching out early and providing care that’s personalized to parents’ …

June 23, 2022
Collaborative care for serious mental health conditions
An innovative telehealth program gives patients direct access to pharmacists …

June 16, 2022
Leadership and innovation to prevent gun injuries and deaths
Kaiser Permanente’s new Center for Gun Violence Research and Education …

May 29, 2022
Gun violence is a public health crisis. A preventable one.
We must do more to prevent gun violence and educate on its health implications …

May 25, 2022
Be a source of comfort and calm
Trusted conversations help youth feel safe when community violence occurs.

May 18, 2022
Initiative improves mental health in gaming community
Newly released results show the Presence of Mind initiative can be an effective …

May 3, 2022
One pill can kill: Understanding the risks of fentanyl
As overdose deaths skyrocket, an addiction medicine specialist explains …

May 2, 2022
How to transform mental health care: Follow the research
We applaud President Biden and Congress as they begin to set policies that …

March 4, 2022
Online quiz helps predict likelihood of teen substance use
Assessment helps parents and caregivers intervene early when kids are at …

October 28, 2021
When things fell apart, telehealth was her lifeline
Stuck at home during the pandemic, a Kaiser Permanente member with autoimmune …

October 27, 2020
Sharing an innovative approach to youth mental health
Don Mordecai, MD, Kaiser Permanente’s national leader for mental health …