Pandemic spurs new approach to diabetes care
A diabetes specialist talks about new trends in providing care, and innovations inspired by the realities of COVID-19.
Diabetes patients can connect with physicians and care teams through virtual visits for safe, frequent check-ins to help manage their condition.
Nearly 1 in 3 Americans either suffers from diabetes or lives with prediabetes, and this population is especially vulnerable during the coronavirus pandemic because they’re at a higher risk of serious complications and death.
John P. Martin, MD, FACP, a director of diabetes management at Kaiser Permanente, spoke about Kaiser Permanente’s approach to diabetes care, including recent changes that minimize face-to-face interactions while still providing high-quality care.
How has diabetes care changed in recent years?
Patients have traditionally looked to their doctor as the key to managing their diabetes, but successfully managing this ongoing health condition relies on an entire care team. Today, the doctor is more of a ringmaster, supervising the coordination of care. There is less need for frequent office visits and more focus on supportive care, such as medication management and the lifestyle and behavioral changes that can help patients control their diabetes.
Much of the daily management of a patient’s diabetes is performed by other health care professionals, such as pharmacists and nurses managing medications, and nutritionists developing meal plans and fitness activities. Kaiser Permanente’s integrated care model, supported by one of the world’s largest electronic health record systems, allows physicians partnered with diabetes care managers to better coordinate care with patients, including monitoring vital signs, adjusting medications, and scheduling regular follow-ups.
How has Kaiser Permanente responded to the challenges presented by the COVID-19 pandemic?
The 2 keys have been virtual care, including both phone and video visits, and increased use of remote patient monitoring. Phone and video visits help our physicians and care teams stay better connected to diabetes patients. And while Kaiser Permanente already had an established remote monitoring program to check on blood sugar levels for diabetes patients, there was a push to enroll more members after the onset of the pandemic to reduce the number of times they needed to physically come in to see the doctor.
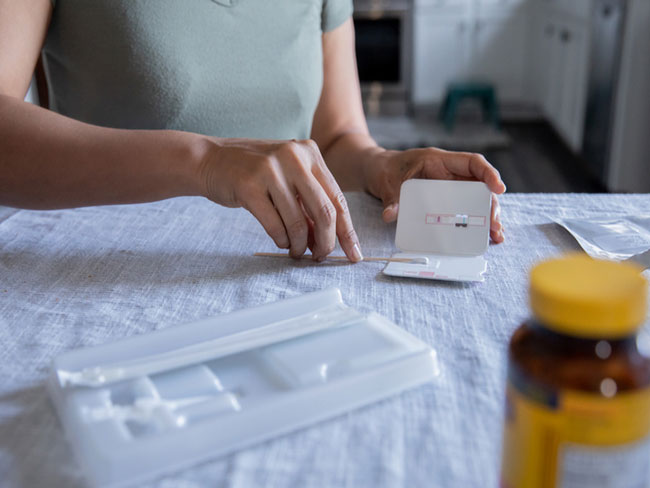
With remote monitoring, patients use a smartphone and a Bluetooth-enabled glucometer to conveniently track and share blood sugar readings directly with their Kaiser Permanente care team. This allows us to recognize early on when we should modify a patient’s treatment and care plan, and lets us proactively adjust medications instead of waiting for the patient to come in for a follow-up visit. Connecting with patients through the remote program helps them avoid forgetting or misunderstanding health care advice and improves their diabetes management outcomes.
What does the future of diabetes care look like?
The COVID-19 pandemic has forced us to look at new models of care, especially for chronic conditions. In the future, diabetes care management should be a blend of safe and frequent electronic interventions balanced with targeted face-to-face encounters. The patient still wants to see the smile of a doctor, and the doctor stills wants that connection with patients, but periodic in-person visits should be supplemented with phone or video for safer, more efficient follow-ups. Regular contact, whether in person or virtually, will help our patients feel supported and set them up for success.