A history of leading the way
Kaiser Permanente’s groundbreaking health plan was opened to all on July 21, 1945. Since then, we’ve evolved the way Americans experience and understand health care and wellness using evidence from scientific research and the latest technology. Explore, learn, and discover how our heritage helps us tackle challenges with one vision in mind: to help our members and communities experience more healthy years.
Establishing core principles
Before we opened to the public, our founders were laying the groundwork for innovation and inclusiveness. A focus on high-quality, affordable care and prevention; integrated hospitals; and the hiring of disabled veterans, women, and people of color set the stage for our future.
July 21, 1945
The Permanente Health Plan opens to the public
Industrialist Henry J. Kaiser partnered closely with founding physician Sidney R. Garfield, MD, to open their proven system of prepaid care to the public in Northern California. Unions viewed the plan as labor-friendly and affordable, and formed a huge and welcome membership base in the formative years. We opened in the Northwest just a few months later. Other formative milestones around this time:
- Our nurses signed what might have been the first nurses labor agreement in the United States with our hospitals in Oakland and Richmond, California.
- The Permanente Medical Group formed in 1948 with 7 physicians, a key step in the evolution of the physician-led leadership model.

January 1, 1948
Kabat-Kaiser Institute opens, offering new polio treatments
We opened Kabat-Kaiser Institute in Washington, D.C, to offer innovative neuromuscular treatments for polio and multiple sclerosis patients. Eventually, we built 2 additional facilities in California, and the institute became the largest nongovernmental civilian rehabilitation program for neurological disorders in the country.
Building our unique workforce
As the health plan established regions in Southern California and Hawaii, the organization continued to expand its diverse pool of highly skilled caregivers, adding more Black doctors and nurses to the staff. Our identity also evolved — we officially adopted the name Kaiser Permanente in 1953.

August 25, 1950
First class of Kaiser Foundation School of Nursing graduates
To help fill a nursing shortage following World War II, we established the Kaiser Foundation School of Nursing. It was open to students of all races and financial backgrounds and became a model for training nurses in a new approach to health care.

Pioneering in multiphasic screening concept
Morris F. Collen, MD, one of the co-founders of The Permanente Medical Group, helped pioneer the multiphasic exam with the support of Dr. Garfield. The exam included procedures and tests that screened for conditions such as diabetes, heart disease, and cancer.
Initially created to screen the influx of longshore workers who’d never had a health plan before, these preventive checkups helped us determine which patients were most in need of care. Dr. Collen made the exams easy for the longshore workers to access by setting them up at the docks.
Photo: Morris F. Collen, MD, a leader in our work to develop and make the multiphasic exams available to our members, standing in front of an exam check-in desk.

Health plan becomes a nonprofit organization
When Kaiser Foundation Health Plan, Inc. was established as an independent nonprofit California corporation, it underscored our mission to provide high-quality, affordable care.
Focused on our mission since the beginning, Henry J. Kaiser had set up The Permanente Foundation as a charitable trust years earlier, to support the hospitals and clinics for the World War II workforce. The Permanente Foundation became Kaiser Foundation Hospitals, a charitable hospital corporation, in the late 1940s.
Photo: Groundbreaking ceremony at the Harbor City Medical Center in 1956. New facilities, such as this one, expanded the Health Plan’s nonprofit services.

January 14, 1957
First hospital to provide employer-sponsored health care
Our Kaiser Foundation Harbor Hospital was the first hospital in the country built for members of an employer-sponsored health care plan. It initially provided care to International Longshore and Warehouse Union employees and their families.
Earlier in the decade, we also built a clinic in Los Angeles to support Retail Clerks Union Local 770; it opened in 1951.
Committing to communities
At a time of social unrest, we further defined our dedication to communities. From tackling public health issues, such as smoking, to providing health education, we took a holistic approach to health. We also continued to expand, this time into Colorado.
Research and technology help advance patient care
While we began publishing medical research in our earliest years, Morris Collen, MD, founded our Department of Medical Methods Research in 1961.
The research institution was a trailblazer in drug safety, health services and policy, genetic research, and more. It also pioneered using technology to store patient medical histories, leading to more informed care and population-based studies.
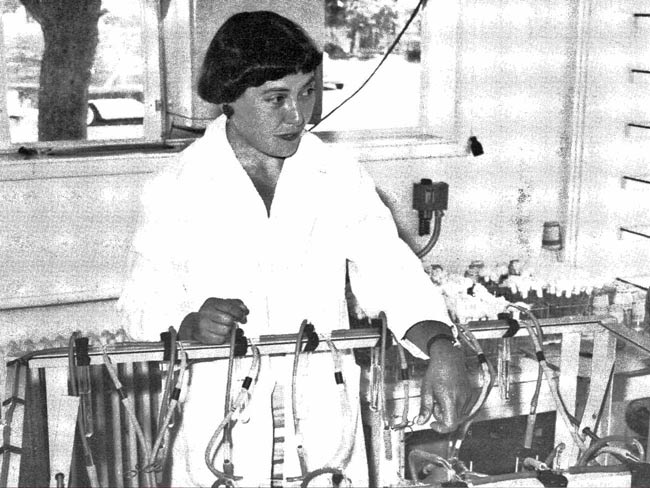
Photo: Dr. Mary Beth Allen, a scientist, and one of the earliest female researchers at Kaiser Permanente, works in the Kaiser Permanente Richmond Laboratory.

September 10, 1962
Unique hospital design helps drive better patient care
To improve care and reduce steps for nurses, our Panorama City Medical Center was designed using Dr. Garfield’s circles of service concept. Nurses’ stations were in the center, ringed by patient rooms, for more efficient patient monitoring.

August 1965
Civil unrest further ignites our community pledge
Community unrest in the Los Angeles area underscored the need for better health and social services in some underserved communities.
We provided critical medical care after the Watts Riots and helped long-term recovery by creating the Watts Counseling and Learning Center, which is still going strong today.
Photo: Bill Coggins, licensed clinical social worker, and director of the Watts Counseling and Learning Center, celebrates its dedication, 1977.
Navigating rapid growth
With the federal government offering our plans to employees, we saw rapid growth and increasing demand for care. We used this opportunity to offer innovative solutions, including adding nurse practitioners to care teams and hitting the road in mobile care vans.

Ahead-of-our-time approach to maternity care and childbirth
Our doctors were among the first to support women giving birth vaginally after having a prior cesarean delivery. There was a long-held “once a cesarean, always a cesarean” belief in the medical community, but Sidney Sharzer, MD, questioned that thinking. He observed countless women scheduled for C-sections arriving at the hospital late in labor and having safe births.
Kaiser Permanente conducted a 5-year study of vaginal births after C-sections in multiple hospitals, which showed reverting to a natural birth process could be successful and safe for many women.
This kind of innovative thinking wasn’t new for Dr. Sharzer. He started a revolution in the childbirth experience a decade earlier when he decided to bring fathers directly into the birthing room. The practice eventually spread across our hospitals and beyond.

Pharmacists take on clinical roles to improve patient health
Innovations in medical and pharmacy practices allowed our pharmacists to work closely with care teams. These partnerships increased the effectiveness of medications, promoted the total health of patients, and supported affordability.
From tracking medication adherence to making sure patients discharged from the hospital have the right medication plan, our pharmacists are a vital part of our integrated care experience.

Modeling the way for HMOs across the country
As health care costs soared in the late 1960s, Kaiser Permanente’s demonstrated affordability was specifically acknowledged when we were recognized as the best health plan model for the groundbreaking Health Maintenance Organization Act, signed into law December 1973. By 1976, all our regions’ health plans were qualified HMOs.
Photo: Lady Bird Johnson recognizes Dr. Garfield and his work as Kaiser Permanente attains HMO status, 1977.

Leading the way in solar power use
Review California AB-1305 compliance disclosures on our greenhouse gas emissions reduction efforts.
At our Redwood City Medical Center, the solar installation for water heating was one the largest of its kind at a U.S. health care facility when it opened. Our commitment to the environment started even earlier, leading to our 2020 milestone of becoming the first health care system in the United States to achieve carbon-neutral status.
Looking beyond the doctor’s office
The HMO legislation of the previous decade paved the way for our expansion into other areas of the United States. We established our Georgia and Mid-Atlantic States regions. As our member base grew, we also recognized the need to use new and creative ways to reach people with important health messages.

Educational Theatre Program’s unique approach to health
It began as a single play for elementary school children. Now, more than 35 years later, our award-winning Educational Theatre continues to educate and inspire individuals and communities to make informed decisions about their health through the power of the arts, storytelling, and human connection.
June 8, 1988
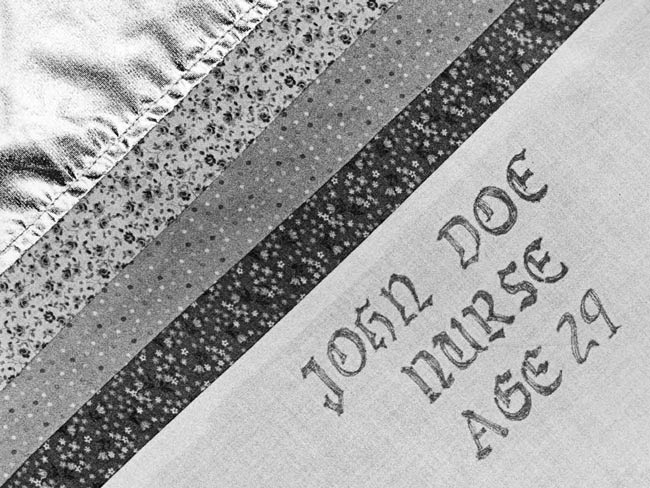
Making improvements in AIDS care
We responded to the unprecedented AIDS crisis by forming an advocacy union and partnering with patients to push for improvements in care — eventually creating an HIV Member Advisory Panel. This became a model program for AIDS care around the country.
Photo: A square from the NAMES Project AIDS Memorial Quilt, which celebrates the lives of people who have died of AIDS-related causes.
Strengthening our culture
We embraced the digital revolution during this decade, launching our first website for members. Our inclusive work culture grew with the expansion of benefits to domestic partners and the establishment of our unique partnership with union-represented employees.
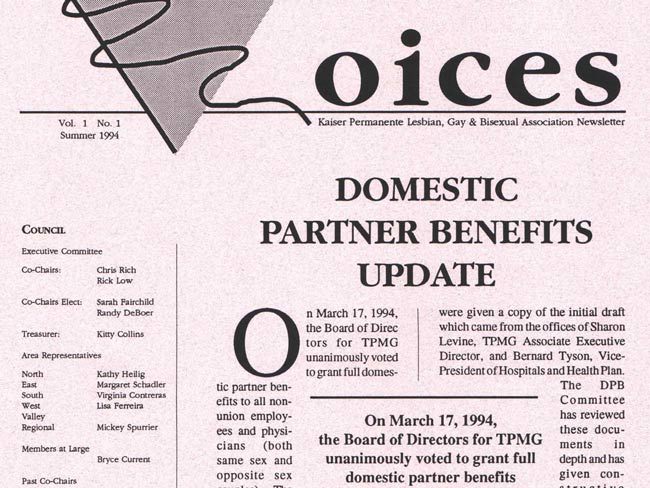
Domestic partners of employees eligible for health benefits
As an early adopter of extending health care benefits to domestic partners of employees, we underscored our commitment to equity, inclusion, and diversity. Our LGBTQ business resource group of employees and physicians was key to making it happen.
July 1997
Historic Labor Management Partnership begins
Kaiser Permanente and many of the unions we worked with entered into a historic partnership that gave workers a stronger voice in decision-making. The Labor Management Partnership encourages collaboration to improve quality, service, and working environments.
Today, the Labor Management Partnership continues to bring together Kaiser Permanente workers, managers, and physicians at all levels of the organization to deliver better care, service, and work life. Learn more about how Kaiser Permanente has long embraced its partnership with labor.

June 1998
Interpreter program helps advance culturally sensitive care
We began to reduce the language barrier in health care with language classes for staff members as early as 1977. Later, we teamed up with City College of San Francisco to create a year-long health care interpreter certification program. The first class of interpreters graduated in 1998 with training in Spanish, Russian, Cantonese, Mandarin, Vietnamese, Cambodian, Laotian, Thai, and more.
Photo: Miriam Amor teaches a Spanish language class for health care practitioners at the Santa Clara Medical Center in 1974.

May 14, 1999
Landmark study on adverse childhood experiences
A Kaiser Permanente study conducted with the Centers for Disease Control and Prevention was the first — and one of the largest — to identify the link between adverse childhood experiences, or ACEs, and health over a lifetime. The study found that children who experience ACEs, specifically abuse, neglect, and household dysfunction, are more likely to have chronic health conditions and engage in risky health behaviors later in life.
Our commitment to preventing ACEs is long term. In 2019, we pledged $2.75 million to new ACEs research, with a goal of identifying the most promising interventions and innovations in preventing and minimizing ACEs to create healthier and more resilient generations in the future.
Affirming our focus on quality
High-quality medical care and technology innovations led the way this decade. Nation-leading prevention programs and specialized care for conditions such as heart disease and certain cancers, along with our leading maternity care cemented our position as a health care innovator.
Improving outcomes with a clinical library
When members visit Kaiser Permanente, they can be sure they’re getting the best, most appropriate care for their condition — care that is based on the latest proven research. That’s because all our doctors, nurses, and clinicians have quick and easy access to our Clinical Library. This central online repository includes 30,000 clinical guidance aids, patient education materials, and other decision-support tools that provide evidence-based references on how to best treat patients.
Clinical Library was established by our Care Management Institute. The institute consistently and reliably improves the quality of care we provide by finding new and better ways of doing things, then spreading those findings to all our care teams. With the library’s help, Kaiser Permanente is regularly recognized as a national leader in quality, safety, and service.

May 16, 2003
Organic farmers market a first at a U.S. hospital
Recognizing the connection between food and health, Preston Maring, MD, started an organic farmers market at our Oakland Medical Center, making fresh, whole foods accessible to more people. Today, there are more than 50 farmers markets at our facilities across the United States.

Introducing industry-leading electronic health records
Our electronic health record set industry standards for electronic clinical information. It created secure, 24/7 access to up-to-date patient records with no geographic boundaries. When the system rollout was completed in 2010, it became the largest private sector electronic health record system in the world. The technology also fueled transformational health research and clinical practices that continue to improve patient outcomes.

PHASE helps prevent heart attacks and strokes
The Preventing Heart Attacks and Strokes Every Day, or PHASE, program was designed for our members with elevated risk of cardiovascular disease, including people who have had a heart attack or stroke, or who have diabetes. The use of a patient registry identifies members who might benefit from intensive risk-factor control, and each patient is treated by a comprehensive care management team.
A 10-year study of this program concluded it was outperforming the nation on controlling 3 cardiovascular risk factors — high blood pressure, abnormal lipid levels, and high blood sugar — for diabetes patients, who make up two-thirds of the program’s participants.
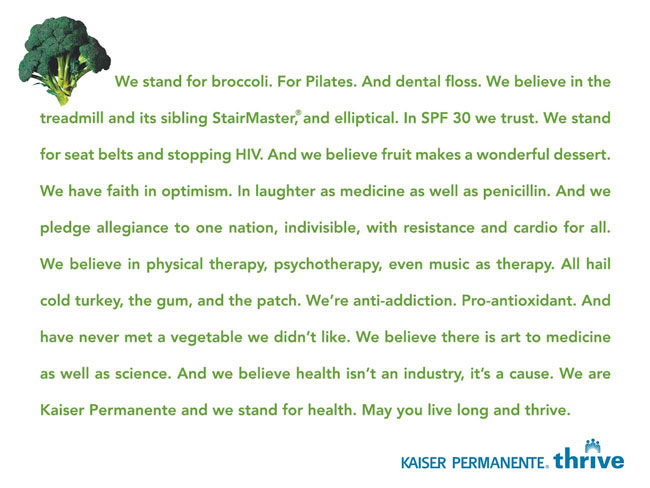
Thrive campaign changes the language of health care
The Thrive campaign perfectly framed our unique approach to health and health care — helping people live healthier lives through preventive medicine, a team approach to care, and a commitment to the total health of our members and our communities.
Photo: In our first Thrive ad we shifted the health care conversation to wellness rather than sickness. The Broccoli Manifesto was our new North Star.

Life-saving alerts added to electronic health record
Our move from paper charts to electronic health records not only improved efficiency and care, it empowered staff members to be advocates for the total health of our members. A tool built into our electronic health records prompts staff members to remind patients when they are due for preventive screenings, such as mammograms, and to help them make appointments. This proactive approach saves lives when it leads to earlier diagnosis and treatment.

Aggressive approach to top killer of hospital patients
Sepsis is a potentially life-threatening condition caused by the body's response to an infection, and it’s the number one cause of death in U.S. hospitals.
We introduced a program that resulted in a threefold increase in the rate of sepsis detection and a 60% reduction in mortality for patients with sepsis.
In 2014, we also developed a neonatal sepsis risk calculator, safely reducing newborn antibiotic use by nearly 50%.

Using exercise as a vital sign to increase physical activity
We became one of the first, and largest, health care organizations to use exercise as a vital sign. That means asking patients about their exercise habits during routine outpatient visits. Their responses are included in their electronic health record along with other traditional vital signs such as blood pressure, pulse, and temperature. This allows doctors to better track, treat, and counsel patients about their total health.

Leading the way in identifying and addressing opioid use
Well before opioid abuse became a national crisis, our doctors and pharmacists were concerned about the potential risks associated with opioids. They were able to detect, analyze, and respond to the opioid crisis faster than many health care providers because of our electronic health record system and connected ecosystem of prescribers and pharmacies.
As early as 2009, we began to implement opioid management programs, and by 2012, they were in place across the organization. These programs help manage how opioids are prescribed, assist patients in tapering down, provide pain management alternatives, and help prevent the drugs from getting into communities.

May 2010
Improving the environment, one supplier at a time
We began requiring medical product suppliers to complete sustainability scorecards in 2010. The scorecards ask each supplier about their environmental commitment, use of potentially harmful chemicals, and recycling policies for their products and packaging. The scorecards allow us to evaluate the sustainability of each item purchased while also encouraging suppliers to provide greener products for the health care industry.
Tackling barriers to health
The decade saw innovative thinking push us to do more. From high blood pressure to homelessness, we tackled the big issues facing health care — recognizing that many factors influence a person’s overall health. We also acquired Group Health Cooperative and its subsidiaries, which became our Washington Region.
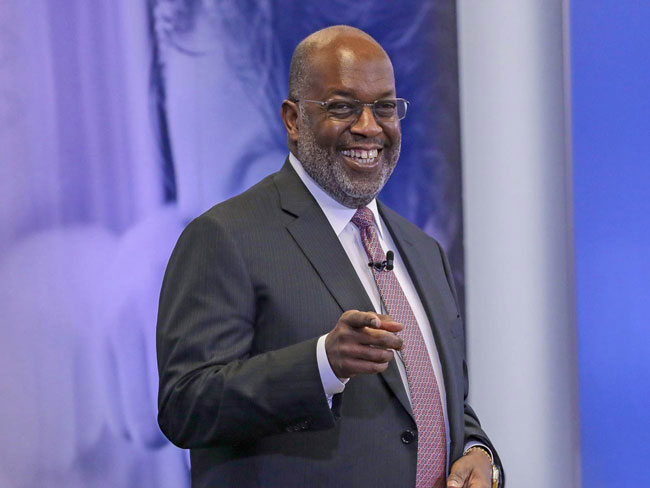
Bernard J. Tyson becomes our first Black CEO
Bernard J. Tyson’s career at Kaiser Permanente spanned more than 3 decades, working his way up through many different roles. He was a trailblazer in health care, health equity, mental health care, and addressing social determinants of health — a man of bold service whose influence was felt around the world. Tyson passed away in 2019.

Research Bank launches nationally to create a healthier future
The Kaiser Permanente Research Bank is one of the largest and most diverse in the world. It’s a collection of health information and blood samples contributed by volunteers and is designed to help the organization better understand how people’s health is affected by their genes, behaviors, and environment.
Our clinical findings using Research Bank data may lead to medical breakthroughs and advancements in care that help our health care professionals improve outcomes and help our members live healthier lives.

Cancer clinical trials program significantly expands
Our cancer research program is one of the largest in the nation. Its size enables the organization to be highly effective in the prevention, diagnosis, and treatment of all aspects of cancer.
In 2014, the program expanded significantly when the National Cancer Institute awarded it $7.3 million. The award was later increased to $10.4 million.
By 2016, Kaiser Permanente had higher patient enrollment in the NCI-sponsored National Clinical Trials Network than any other program in the United States.

October 2015
First successful transcarotid artery revascularization
World-renowned vascular surgeon Peter Schneider, MD, working at Kaiser Permanente in Hawaii, successfully performed the first transcarotid artery revascularization, which allowed him to treat a patient's blocked artery with minimal risk for nerve injury and heart trauma.
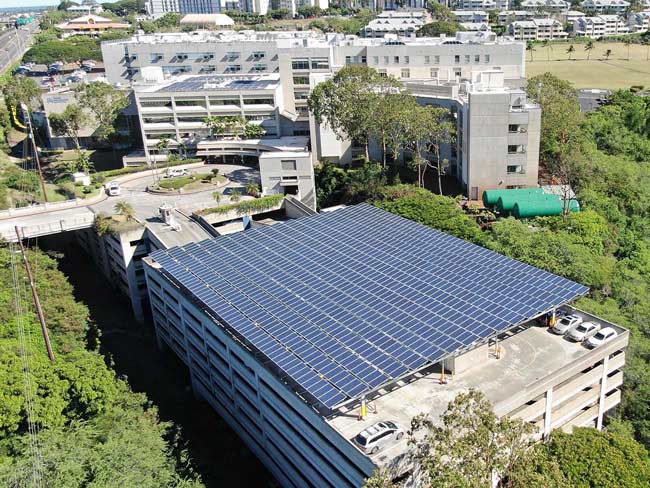
Setting ambitious, industry-leading environmental goals
Review California AB-1305 compliance disclosures on our greenhouse gas emissions reduction efforts.
Our commitment to sustainability dates back to the 1960s. As an early leader in recycling programs, solar panel use, and other conservation approaches, we took our most ambitious stance in 2016.
To reduce our environmental impact and help restore and revitalize our communities by 2025, Kaiser Permanente committed to becoming carbon net neutral; recycling, reusing, or composting 100% of our non-hazardous waste; and taking other big steps to set an example for the health care industry and positively impact the environment for future generations.
December 2017
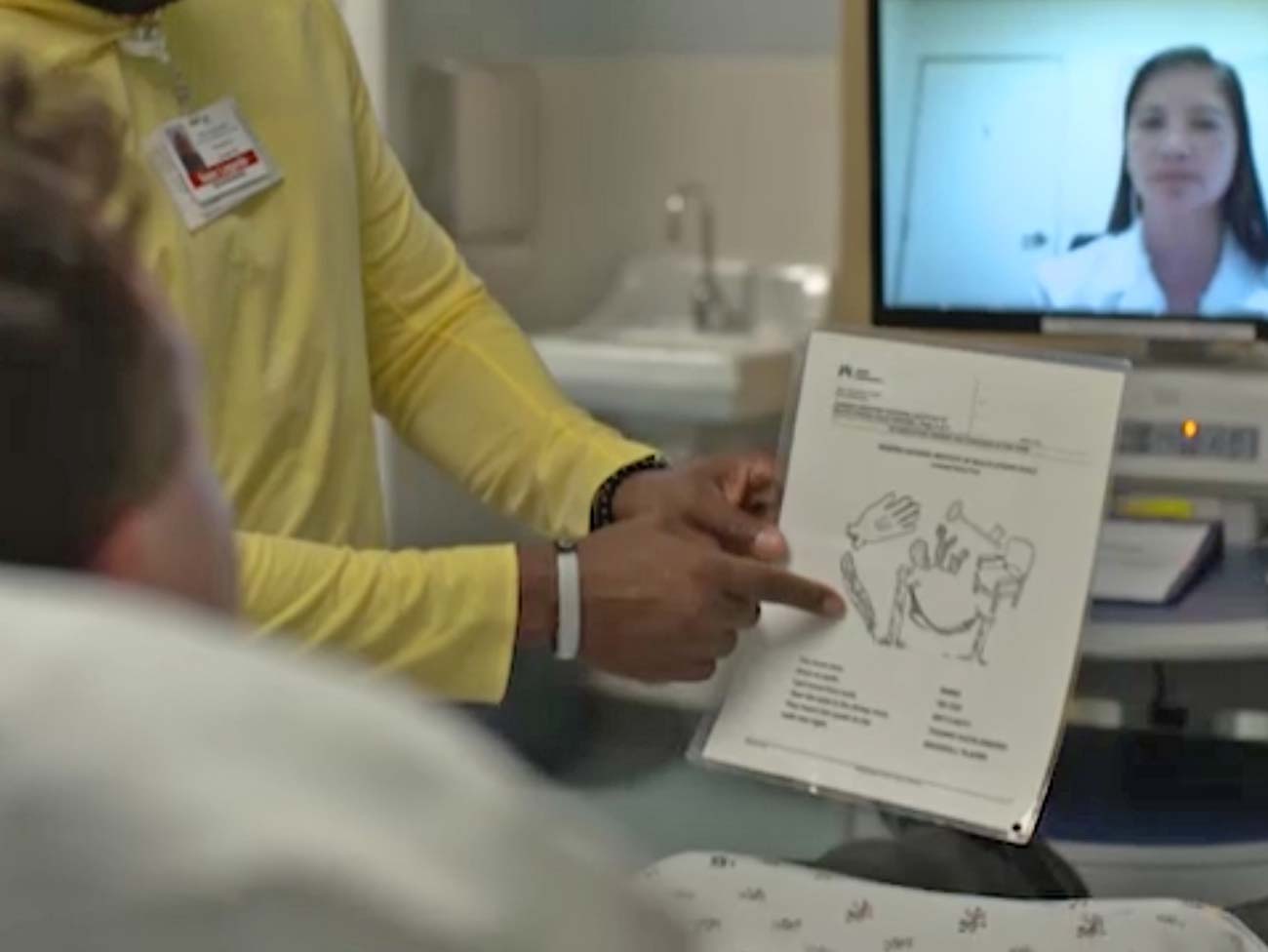
Research shows we’re better at saving stroke patients’ lives
Our evidence-based stroke response program ensures patients receive clot-busting medication more than twice as fast as the national average. The telehealth approach includes an on-call neurologist who examines patients via videoconferencing for faster diagnosis.

Leading the nation in controlling blood pressure
Our deliberate focus on prevention and treatment helps us lead in blood pressure control. For the sixth year in a row, we were the national leader for high blood pressure control, according to the 2018 NCQA Quality Compass.

May 2018
Tackling housing, a critical driver of health
Our long-standing focus on the total health of our communities continued with a $200 million investment in programs and partnerships to address housing stability and homelessness. The investment inspired action from other industry leaders to help solve this crisis.

October 2019
World’s first double LEED certified hospital
Review California AB-1305 compliance disclosures on our greenhouse gas emissions reduction efforts.
Our San Diego Medical Center opened in 2017 and was certified at the Leadership in Energy and Environmental Design, or LEED, Platinum level.
In 2019, it achieved LEED for Existing Buildings: Operations and Maintenance Platinum certification, making the facility the first double LEED Platinum hospital in the country.
Leading with strength and resilience
The beginning of this decade has included many unprecedented moments. Kaiser Permanente is proud to help lead during challenging times and will continue to evolve with the world around us.

April 2020
As telehealth needs soar, our robust systems deliver
With stay-at-home orders in place in nearly every U.S. state due to the COVID-19 pandemic, member telehealth visits reached all-time highs. Within weeks, virtual care visits rose from about 15% of all visits to about 80%, including more than 30,000 a day via video.
In addition, our mail-order pharmacy dispensing increased to its highest percentage and volume in our history — 3.6 million prescriptions in April 2020 — a 61% jump from the previous month.
Our solid technological infrastructure allowed us to rapidly rise to this occasion, ensuring patient access and safety during a challenging time.

May 2020
Unique mental health initiative reaches gamers and fans
Suicide is the second-leading cause of death among people aged 10 to 34, and half of mental health conditions begin by age 14. That’s why we teamed up with esports organization Cloud9 to launch a first-of-its-kind mental health and wellness initiative that meets youth and young adults where many are spending their time — online gaming.
Called Presence of Mind, the initiative aims to increase mental health awareness among online gamers and fans, reduce stigma, and encourage teens and young adults to prioritize their well-being. It’s one of the many ways we are working to help build a stronger foundation of mental and emotional health across the nation.
June 2020
Taking action to fight racism and promote equity
Systemic racism and a lack of economic opportunities for communities of color, especially Black communities, prevent many from achieving total health.
In response to this persistent national issue and to further our longstanding commitment to equity and inclusion, we announced a series of actions, including:
- A $60 million investment partnership to strengthen and support businesses led by Black and other underrepresented individuals.
- $15 million in grant dollars to increase access to formal training, business networks, and recovery and growth capital to help businesses led by Black and other underrepresented groups overcome systemic economic disadvantage.
- An additional $25 million in grants to build upon our work addressing adverse childhood events and trauma and to support grassroots efforts to end systemic racism.
- Increased efforts within our organization to enhance workplace inclusiveness and supplier diversity.

July 27, 2020
School of medicine welcomes its inaugural class
The Kaiser Permanente Bernard J. Tyson School of Medicine in Pasadena, California, welcomed its first class of 50 future physicians. The school is dedicated to educating diverse students who will become outstanding clinicians and skilled advocates for equity and the health of their patients and communities.