Speed saves lives: Fast stroke treatment key to survival
When a stroke happens, minutes matter, and Kaiser Permanente treats strokes with clot-busting medication more than twice as fast as the national average.
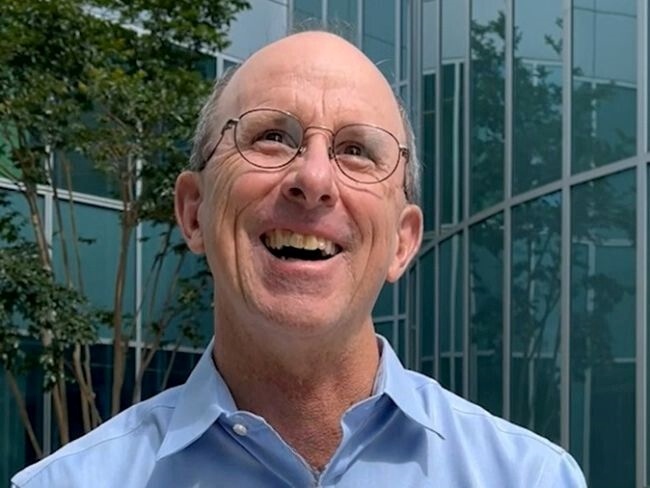
Ken Dito, a long-time Northern California radio sportscaster and journalist, always kept an eye on the clock to avoid missing deadlines. When he recently suffered a stroke, he found himself again racing against the clock, but this time the stakes were higher. He was on deadline to save his life.
“When a stroke happens, minutes matter,” said Mai Nguyen-Huynh, MD, vascular neurologist at Kaiser Permanente Diablo Service Area and research scientist with the Kaiser Permanente Division of Research.
Immediate treatment increases the chance of survival and decreases the likelihood of disability. Studies show that Kaiser Permanente in Northern California provides patients with lifesaving treatment faster than the national average.
“Nearly a million people each year are affected by this dangerous medical emergency that blocks the flow of blood supply to the brain,” Dr. Nguyen-Huynh said.
It started as a routine golf outing
Dito, 85, recalls getting out of his car at a local golf course and grabbing his clubs out of the trunk. Then, everything went dark. Fortunately, people nearby called an ambulance that rushed Dito to the Kaiser Permanente South San Francisco Medical Center.
Dito benefited from Kaiser Permanente’s integrated, meticulously choreographed telestroke program, which reduces the time from arrival at the medical center to administration of clot-busting medication.

Ken Dito can’t recall much from the day he suffered a stroke, but he is grateful for the cutting-edge care he received from Kaiser Permanente, which saved his life.
The process actually begins before patients arrive at the medical center. As soon as paramedics or other medical staff alert the medical center that someone may be having a stroke, the teleneurologist on call is notified of a potential stroke alert. The local emergency department team — which includes but is not limited to an emergency department physician, nurses, radiology and lab technicians, and transport staff — starts preparing for the patient’s arrival. Once in the medical center, the patient is swiftly assessed virtually by a remote neurologist. If the patient qualifies, clot-busting medication, also known as an intravenous thrombolytic, is given to improve the chance of survival and minimize permanent disability.
“These thrombolytics dissolve the stroke-causing clot and they restore blood flow to the brain,” Dr. Nguyen-Huynh added. “They are strongly associated with better functional outcomes for stroke patients.”
When it comes to receiving thrombolytics, the American Heart Association and American Stroke Association recommend a “door-to-needle” time of 60 minutes or less for a patient to have the best possible outcome. Studies show that fewer than 30% of patients in the United States who experience an acute ischemic stroke are currently being treated within this window.
Kaiser Permanente has been at the forefront of advancing stroke treatment and is an industry leader in reducing door-to-needle times. In 2022, 38 Kaiser Permanente hospitals received the American Heart Association’s “Get With The Guidelines®-Stroke Gold Plus Quality Achievement Award,” given to hospitals recognized for high-quality stroke care.
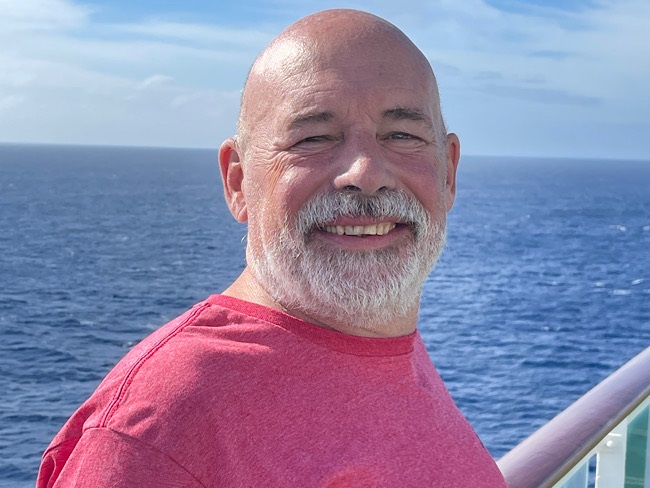
In Dito’s case, after he received the medication he was rushed to the Kaiser Permanente Redwood City Medical Center, an accredited Comprehensive Stroke Center. There, he received treatment from Sean Cullen, MD, a neurointerventional radiologist, and his team.
“It was a significant stroke. He was completely unable to speak and totally paralyzed in the right arm and leg,” Dr. Cullen said. “He not only had a blood clot in the brain but also a clot blocking the neck’s carotid artery that leads to the brain.”
Dr. Cullen surgically removed both clots and quickly restored blood flow to Dito’s brain, a procedure that lasted just 14 minutes.
Quickly getting back to normal
Less than an hour after the surgery ended, Dr. Cullen visited Dito in his hospital room.
“He was awake, oriented, and speaking normally,” said Dr. Cullen. “I’m so proud of the stroke care system that we have here at Kaiser Permanente. He was very lucky to be diagnosed quickly and sent here.”
Dito is grateful for the care he received.
“The doctors and nurses at Kaiser Permanente, they saved my life,” Dito said. “I’m even back to playing golf.”