Stroke rate 4 times higher in Black adults than whites
Kaiser Permanente research shows the need to raise awareness about the dangers of high blood pressure.
PRESS RELEASE
Contact: Susan Rochman
susan.l.rochman@kp.org
415-265-2418
Contact: Kerry Sinclair
ksinclair@webershandwick.com
310-710-0321
OAKLAND, Calif. — Black middle-aged adults had an incidence rate of stroke 4 times higher than that of white middle-aged adults, according to a Kaiser Permanente study published March 29 in Hypertension.
The large national prospective study highlights the need to raise awareness among young and middle-aged Black adults about the impact of high blood pressure, called hypertension, on stroke, the research team said.
“What we found striking in this study was that the incidence of stroke began to increase rapidly starting at around age 40 for Black adults,” said the study’s co-author Jamal S. Rana, MD, PhD, an adjunct investigator with the Division of Research at Kaiser Permanente in Northern California, and cardiologist with The Permanente Medical Group. “It is well known that Black adults have higher rates of hypertension in general, but the fact that their blood pressure levels are starting to increase at such an early stage in life is concerning.”
The research used data collected in the Coronary Artery Risk Development in Young Adults study. Launched in 1985, CARDIA enrolled 5,115 Black and white women and men ages 18 to 30 at research hospitals in 4 cities. Blood pressure measurements and other tests were performed when participants entered the study, and were conducted every 5 years, with 2 additional exams at years 2 and 7.
This analysis included data collected on 5,079 participants starting from 1990 through 2018. In 1990, the Black adults already had higher rates of elevated blood pressure and diagnosed hypertension than the white adults. By 2018, 100 people in the study had had a stroke, at a median age of 49.8. The stroke incidence rate was 29 per 100,000 person-years for white adults compared with 120 per 100,000 person-years for Black adults — a rate more than 4 times higher. A person-year is a measurement that takes into account the number of people in a study and the amount of time each person spends in the study. The analysis also took into account other risk factors for stroke, such as smoking, diabetes, high cholesterol, obesity, lack of physical activity, and excessive alcohol use.
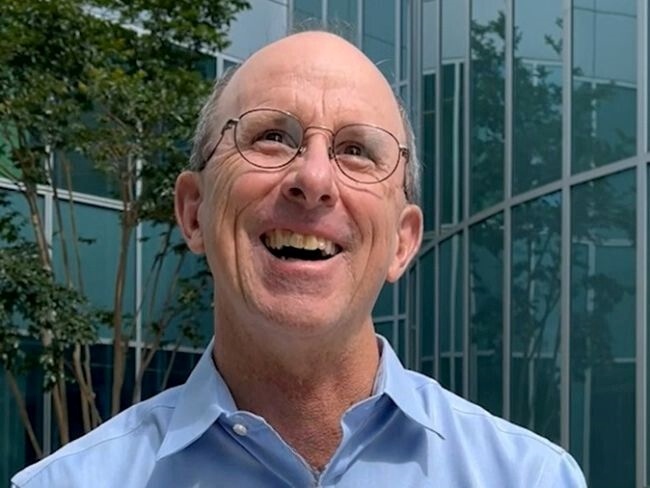
“This study confirms that it’s not only whether you have high blood pressure but how long you have had high blood pressure and how long the damage to the blood vessels has been occurring that matters,” said the study’s senior author Stephen Sidney, MD, MPH, a research scientist at the Kaiser Permanente Division of Research. “It also tells us that interventions need to be put in place to prevent high blood pressure from ever even occurring.”
The study’s first author Yariv Gerber, PhD, a professor of epidemiology and head of the School of Public Health at Tel Aviv University in Israel, conducted the research while on a sabbatical at the Kaiser Permanente Division of Research. “We demonstrated that the association of high blood pressure with stroke varies with age, strengthening from young adulthood to midlife,” said Dr. Gerber. “The association was also dynamic, with the most recent measurement most strongly associated with subsequent stroke risk. This stresses the need for early public health interventions to maintain optimal blood pressure levels in young adulthood, particularly in high-risk Black young adults.”
Previous research suggests young adults age 18 to 39 in the United States are less aware than adults age 40 and older about what their blood pressure numbers mean and why it is important to keep blood pressure low. “Anytime you talk about abnormal blood pressure, the biggest challenge is always that people are not feeling it in real time,” said Dr. Rana. “It is not until a person’s blood pressure has been out of control for a prolonged period of time that they feel any symptoms. Our goal should be to have people proactively think about blood pressure control.”
The study was supported by the National Heart, Lung, and Blood Institute.
Co-authors include Mai N. Nguyen-Huynh, MD, MAS, of the Division of Research; David R. Jacobs Jr., PhD, of the University of Minnesota; Yuichiro Yano, PhD, of Duke University; Deborah Levine, MD, MPH, of the University of Michigan, Ann Arbor; Joao A.C. Lima, MD, MBA, of the Johns Hopkins School of Medicine; Jared P. Reis, PhD, of the National Heart, Lung, and Blood Institute; Lihui Zhao, PhD, and Kiang Liu, PhD, of Northwestern University; and Cora E. Lewis, MD, MSPH, of the University of Alabama.
About Kaiser Permanente
Kaiser Permanente is committed to helping shape the future of health care. We are recognized as one of America’s leading health care providers and not-for-profit health plans. Founded in 1945, Kaiser Permanente has a mission to provide high-quality, affordable health care services and to improve the health of our members and the communities we serve. We currently serve 12.4 million members in 8 states and the District of Columbia. Care for members and patients is focused on their total health and guided by their personal Permanente Medical Group physicians, specialists, and team of caregivers. Our expert and caring medical teams are empowered and supported by industry-leading technology advances and tools for health promotion, disease prevention, state-of-the-art care delivery, and world-class chronic disease management. Kaiser Permanente is dedicated to care innovations, clinical research, health education, and the support of community health.